Arterial blood gas analysis and interpretation in anesthetized patients
An introduction to the principles of clinical blood gas analysis and interpretation--including two case examples.
In the past, blood gas analysis and interpretation were performed primarily at university and large referral hospitals. The main argument against using blood gas analysis to guide case management in private practice was the cost of purchasing and maintaining a bench-top blood gas analyzer. With the availability of relatively inexpensive point-of-care units (e.g. VetScan i-STAT 1—Abaxis; Irma 2000SL—Diametrics Medical; VetStat Electrolyte and Blood Gas Analyzer—IDEXX), blood gas analysis and interpretation have become more common. This article introduces veterinarians to the principles of clinical blood gas analysis and interpretation and provides two case examples (see the Related Links "Case example 1: A border collie with a possible foreign body" and "Case example 2: A diabetic husky with a fibrosarcoma" below).

Comstock Images/Getty Images
SAMPLE COLLECTION
Blood gas analysis begins with the collection of the sample. Arterial blood is preferred when assessing respiratory and metabolic status, but venous blood may be useful for the assessment of some metabolic disturbances such as those that occur during severe diarrhea, vomiting, and some toxin exposures. Free-flowing lingual venous blood can sometimes be used to estimate arterial blood gas values in anesthetized animals when arterial blood is unobtainable.1 Common sites for arterial blood collection in dogs and cats include the dorsal pedal artery, femoral artery, or lingual artery. But any large superficial artery may be used.
Sample collection is usually performed with a 1- or 3-ml syringe with a 21-ga or smaller needle. The sample should be collected into a heparinized syringe, which is usually just a syringe that has been filled with heparin and then emptied. This process coats the inside of the syringe barrel and the needle hub. Alternatively, syringes containing powdered heparin specifically designed for arterial blood collection are commercially available. Collect enough blood (about 1 ml) to prevent the heparin from diluting the blood markedly. Expel all visible air from the syringe after sample collection. If the sample will not be analyzed immediately, cap it and place it on ice until it is run.2 However, if accurate partial pressure of oxygen in arterial blood (PaO2) values (< 10 mm Hg change) are important, samples collected into plastic syringes should be run within 10 minutes, even if placed on ice.3,4
Common errors associated with improper sample collection and storage are
1. If the sample is left uncapped for a prolonged period, the partial pressure of carbon dioxide in the arterial blood (PaCO2) and the PaO2 may decrease. The PaO2 may increase if the sample PaO2 is less than the partial pressure of oxygen in the room (e.g. venous blood).
2. If the sample is unchilled for a long period, cellular metabolism will continue, the PaO2 will decrease, and the PaCO2 will increase.
3. If the blood is not anticoagulated, the sample will clot in the system and cause an error.
Before a blood gas analysis can be interpreted, the conditions the patient was exposed to need to be considered. The blood gas machine often requires input of the fraction of inspired oxygen (FiO2) and body temperature to calculate alveolar-arterial (A-a) gradients and temperature corrected values, respectively. It is also important to know this information when you interpret the blood gas values clinically.
ANALYZER OUTPUTS
In this article, I focus on interpreting the PaCO2, PaO2, bicarbonate (HCO3 -), base excess, and alveolar-arterial oxygen difference (AaDO2) values. Normal values for several of these parameters in dogs, cats, and people are given in Table 1.
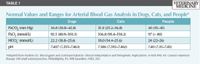
Table 1: Normal Values and Ranges for Arterial Blood Gas Analysis in Dogs, Cats, and People
Additionally, many blood gas analyzers also measure sodium, potassium, and calcium; total plasma protein can be measured with a refractometer or other technique. This additional information allows the calculation of the anion gap or other ionic differences that can provide insight into the metabolic origin of some acid-base disturbances.5,6 These nontraditional approaches to assessing acid-base balance are not routinely used to manage anesthetized patients during surgery, and, thus, they will not be covered here. However, these approaches will be encountered in the context of metabolic acid-base disturbances in critical care and internal medicine cases. A discussion on anion gap and strong ion difference theory is beyond the scope of this article.
PaCO2
The PaCO2 increases when alveolar minute ventilation is decreased and vice versa. When the PaCO2 increases, ventilation is said to be depressed (i.e. hypoventilation). Most anesthetic drugs (e.g. opioids, inhalant anesthetics, propofol) are respiratory depressants; thus, the PaCO2 usually is increased during anesthesia unless ventilation is controlled. Carbon dioxide—not oxygen—is the main stimulus for respiration during anesthesia in normal patients.
PaO2
The PaO2 is the partial pressure of oxygen dissolved in the arterial plasma. Alone, this value does not tell you the oxygen content in the blood. Hemoglobin is the major carrier of oxygen in blood but is not the carrier of dissolved oxygen in plasma; thus, a hematocrit or hemoglobin concentration is also required before estimating the oxygen content. The relationship between the PaO2 and oxygen content is estimated by the equation7:
Oxygen content (ml/dl) =
(hemoglobin concentration [g/dl] X
hemoglobin saturation [%] X 1.3) +
(0.003 X PaO2)
The value 1.3 in this equation is the amount of oxygen that can combine with 1 g of human hemoglobin. It is commonly given as a constant, but it varies among species. This equation calculates the amount of oxygen carried by the hemoglobin (hemoglobin concentration [g/dl] X hemoglobin saturation [%] X 1.3) and the amount carried as dissolved oxygen in the plasma water (0.003 X PaO2).
Anemic animals may have high PaO2 values but little oxygen content (capacity) because their hemoglobin concentrations are reduced. Hemoglobin saturation measured from an arterial blood sample (SaO2) is a calculated value based on the oxyhemoglobin dissociation curve. Alternatively, hemoglobin saturation can be measured with a pulse oximeter, and oxygen content can be estimated without blood gas analysis.
Normal PaO2 values will vary with FiO2 and can be calculated by using the alveolar gas equation. However, an estimate can be made quickly by multiplying the inspired oxygen percentage by five. For example, when breathing room air (21% oxygen), a normal PaO2 should be around 100 mm Hg. For a patient receiving 100% oxygen, the PaO2 should be closer to 500 mm Hg. Hypoxemia (low PaO2) becomes a critical concern in most anesthetized animals when it falls below 60 mm Hg because SaO2 and oxygen content fall precipitously below this PaO2 value.7
Bicarbonate concentration
The bicarbonate (HCO3 -) concentration is calculated from the PaCO2 value by using a mathematical relationship programmed into the analyzer. Some machines report actual and standardized values. Standardized values are corrected to 98.6 F (37 C), a PaCO2 of 40 mm Hg, and normal oxygenation. Bicarbonate is one of the major acid buffering compounds in the body. When bicarbonate is altered, body pH is altered or compensatory mechanisms are activated.
TCO2
Total carbon dioxide is given, but the total carbon dioxide in the blood is largely a function of the actual bicarbonate concentration. Usually 95% of the total carbon dioxide reported is due to the actual bicarbonate concentration. It is not an independent measure of acid-base status because it depends on actual bicarbonate, which in turn depends on the PaCO2.
Base excess
Base excess is the amount of strong acid needed to titrate the pH of 100% oxygenated human blood to 7.4 at 98.6 F (37 C) and at a PaCO2 of 40 mm Hg.8 This parameter is often referred to as a base deficit but is also frequently called the negative base excess. Normal base excess for a person is 0 +/- 2, but base excess in veterinary patients will vary more depending on the species. Base excess is influenced by the total serum protein concentration and will decrease about 2.9 mEq/L for every 1 g/dl increase in total protein concentration. Base excess gives an indication of the metabolic component of acid-base disturbances and is generally unaffected by changes in the PaCO2.
Base excess values can be used to calculate a replacement bicarbonate dose to correct metabolic acidosis. The formula is usually given as
bicarbonate (mmol) =
body weight (kg) X base excess
(mmol/L) X 0.3 (or some other factor)
The factor 0.3 is used for acute corrections because bicarbonate distributes to the extracellular fluid acutely. When long-term bicarbonate therapy is indicated, other factors such as 0.6 are sometimes used because bicarbonate therapy is usually targeted to the total body water (a larger volume of distribution). During anesthesia we correct acutely, so 0.3 is most commonly used.
When bicarbonate is given to patients, it is often administered slowly. Only 25% to 33% of the calculated amount is given in any one dose because when acids are neutralized by bicarbonate, carbon dioxide is rapidly produced. This carbon dioxide must be removed (usually by the lungs), or severe hypercapnia and paradoxical cerebral acidosis may result. Anesthetized patients usually have some degree of respiratory depression and are unable to excrete large amounts of carbon dioxide as efficiently as conscious animals are.
AaDO2
The alveolar-arterial oxygen difference (AaDO2 or A-a gradient) is an indication of the difference in oxygen partial pressure between the gas in the alveoli and the blood leaving the left ventricle (assumed to be the same as the blood in the pulmonary capillaries). This difference is most useful to indicate the degree of impairment of oxygen uptake due to factors such as pulmonary disease, atelectasis, or other causes of ventilation-perfusion mismatching during anesthesia. Normal A-a gradients are generally less than 25 mm Hg in room air (FiO2 ~ 0.21) but may increase at higher FiO2 values.
SIMPLIFIED APPROACH TO BLOOD GAS INTERPRETATION
Arterial blood gas analysis will provide two separate but related pieces of clinical information. First, it provides information on the respiratory status of the patient (PaO2, PaCO2, A-a). Second, it gives you information on the acid-base status of the patient (pH, HCO3 -, base excess).
Respiratory status
Oxygen is less diffusible than carbon dioxide, so impairments to diffusion will cause the A-a gradient to increase (Table 2). A more common cause of increased AaDO2 during anesthesia is the mixing of nonoxygenated blood with oxygenated blood (e.g. shunting or ventilation-perfusion [V/Q] mismatch). Unoxygenated hemoglobin will mix with oxygenated hemoglobin and steal oxygen away until both are equally saturated. Because of the shape of the oxyhemoglobin dissociation curve, the PaO2 will not directly tell you the magnitude of the arterial-venous mixing. During anesthesia, it is common to have increased V/Q mismatch and A-a gradients, especially in large animals.

Table 2: The Five Causes of Hypoxemia in Anesthetized Patients
Carbon dioxide production is usually relatively constant during anesthesia. Since most of the carbon dioxide produced is excreted through the lungs, changes in minute ventilation will alter measured PaCO2. When minute ventilation is doubled, the PaCO2 will decrease by about 50%. When minute ventilation is halved, the PaCO2 will about double. This relationship is worth knowing because it allows an anesthetist to adjust a ventilator to maintain a desired PaCO2 during anesthesia.
Acid-base status
The traditional approach to assessing acid-base status is based on the Henderson-Hasselbalch equation. The PaCO2 is an independent measure of the respiratory component of the acid-base balance, while extracellular base excess is an independent measure of the nonrespiratory (metabolic) component of acid-base balance, and the pH is used as a measure of overall acid-base status.
Four primary acid-base disturbances are possible: respiratory acidosis with increased carbon dioxide, respiratory alkalosis with decreased carbon dioxide, metabolic acidosis with decreased base excess, and metabolic alkalosis with increased base excess and HCO3 - (Table 3). Compensation may occur to reduce the magnitude of the primary abnormality, but it never results in overcorrection.

Table 3: Characteristics of Primary Acid-Base Disturbances
Acid-base disturbances are often corrected before or are tolerated during anesthesia. It may be less problematic to correct chronic abnormalities slowly rather than correcting them during a short anesthetic-surgical procedure. Acute respiratory depression or hypoxia is common during anesthesia and is usually corrected rapidly.
Three steps can be used to quickly assess the acid-base status of anesthetized patients.
Step 1. The first step is determining the primary disturbance. The pH indicates the direction of the primary condition. If the pH decreases, the primary condition is causing acidosis. If the pH increases, the primary condition is causing alkalosis.
Step 2. The second step is to determine if the primary condition has a respiratory component. If the primary condition is acidosis with a respiratory component, the PaCO2 should increase. If the PaCO2 were decreased, you could conclude that there is respiratory compensation, which can be partial or complete depending on the duration of the condition. Compensation takes some time and may not be obvious if the sample is collected early in the acid-base derangement.
If the primary condition is alkalosis with a respiratory component, the PaCO2 should be decreased. If PaCO2 is increased, it indicates respiratory compensation.
Step 3. The next step is to determine if the primary condition has a metabolic component. If the primary condition is acidosis with a metabolic component, the base excess and HCO3 - should be decreased. If it were increased, that would indicate metabolic compensation.
Conversely, if the primary disturbance is alkalosis with a metabolic component, then the base excess should be increased. A base excess and HCO3 - decrease would indicate metabolic compensation. Again, sufficient time is necessary for compensation to occur.
Interpretation
Acid-base disturbances are not primary diseases but are signs of an underlying condition that should be diagnosed and corrected. For example, treating metabolic acidosis with bicarbonate (or with another alkalinizing agent) without treating the underlying cause will only mask the clinical signs and may not improve patient survival. Likewise, treating respiratory acidosis with an alkalinizing agent is contraindicated. The correct treatment for respiratory acidosis is increasing ventilation. The addition of bicarbonate would only worsen the hypercarbia if the ventilation could not compensate.
Some patients have mixed acid-base disturbances. That is, they have two or more simultaneous respiratory or metabolic conditions associated with the primary disturbance (e.g. simultaneous respiratory acidosis and metabolic acidosis). A mixed acid-base disturbance is particularly common during anesthesia when a patient has preexisting metabolic acidosis. When the patient is anesthetized and respiratory depression occurs, the PaCO2 will increase and any respiratory compensation that had occurred will be replaced by respiratory acidosis. Patients may also have two or more metabolic diseases occurring simultaneously. An example would be diabetic ketoacidosis with a superimposed lactic acidosis. Another possible condition is the presence of two or more disorders that may have opposite effects on the pH (offsetting), resulting in a reduction in the magnitude of the primary disturbance.
When a primary metabolic disturbance occurs, it is often worthwhile to analyze the blood gas results with nontraditional methods (i.e. also calculate the anion gap and strong ion difference) and interpret the results in the context of the clinical picture such as previous exposure to toxins, severe dehydration, or electrolyte abnormalities secondary to gastrointestinal disease. Other less traditional methods that are better suited to characterize metabolic disturbances include the strong ion model and simplified strong ion model. These methods may be more appropriate for the acid-base assessment of patients with metabolic disturbances, such as lactic acidosis or renal disease. Metabolic disturbances are usually more long-term and complex than are anesthesia-induced respiratory disturbances.
The effect of plasma constituents. It is important that you understand the influence of plasma constituents on a patient's apparent acid-base balance. Although that cannot be adequately addressed in one article, I hope you appreciate that common protein, bicarbonate, and electrolyte changes can alter a patient's overall acid-base status.9
For example, dilutional acidosis can occur after administration of an alkali-free chloride-containing solution (0.9% sodium chloride solution), which causes volume expansion of the extracellular fluid. Dilutional acidosis occurs because chloride is rapidly absorbed in the kidney and causes a decrease of HCO3 -. A solution containing less chloride (0.45% sodium chloride solution) would reduce this effect.
The opposite occurs when free water is lost and the extracellular fluid constituents are concentrated. In this instance, sodium is often elevated, producing hypernatremic, or contraction, alkalosis. In patients with severe diarrhea, bicarbonate is lost in excess of chloride, leading to hyperchloremic acidosis. This acidosis may be confounded further by lactic acidosis if tissue perfusion is reduced because of severe volume loss and dehydration.
Kurt A. Grimm, DVM, MS, PhD, DACVA, DACVCP
Veterinary Specialist Services
P.O. Box 504
Conifer, CO 80433
REFERENCES
1. Pang DS, Allaire J, Rondenay Y, et al. The use of lingual venous blood to determine the acid-base and blood-gas status of dogs under anesthesia. Vet Anaesth Analg 2009;36(2):124-132.
2. Brito MV, Cunha IC, Aragón MG, et al. Effects of blood storage on ice in biochemical and arterial blood gas analysis of rats. Acta Cir Bras 2008;23(5):462-468.
3. Picandet V, Jeanneret S, Lavoie JP. Effects of syringe type and storage temperature on results of blood gas analysis in arterial blood of horses. J Vet Intern Med 2007;21(3):476-481.
4. Knowles TP, Mullin RA, Hunter JA, et al. Effects of syringe material, sample storage time, and temperature on blood gases and oxygen saturation in arterialized human blood samples. Respir Care 2006;51(7):732-736.
5. Muir WW, deMorais H. Acid-base balance: traditional and modified approaches. In: Thurmon JC, Tranquilli WJ, Benson GJ, eds. Lumb and Jones' veterinary anesthesia. 3rd ed. Baltimore, Md: Williams & Wilkins, 1996.
6. Constable PD. Clinical assessment of acid-base status. Strong ion difference theory. Vet Clin North Am Food Anim Pract 1999;15(3):447-471.
7. Haskins SC. Monitoring anesthetized patients. In: Tranquilli WJ, Thurmon JC, Grimm KA, eds. Lumb and Jones' veterinary anesthesia and analgesia. 4th ed. Ames, Iowa: Blackwell Publishing, 2007.
8. Muir WW, de Morais HAS. Acid-base physiology. In: Tranquilli WJ, Thurmon JC, Grimm KA, eds. Lumb and Jones' veterinary anesthesia and analgesia. 4th ed. Ames, Iowa: Blackwell Publishing, 2007.
9. DiBartola SP. Fluid therapy in small animal practice. Philadelphia, Pa: WB Saunders, 1992.
ADDITIONAL READING
1. Bailey JE, Pablo LS. Practical approach to acid-base disorders. Vet Clin North Am Small Anim Pract 1998;28(3):645-662.