A challenging case: Painful periocular swelling in a cat
An ophthalmic examination provides valuable clues for diagnosing an uncommon disorder with mostly nonspecific signs.
A 4-year-old 10.1-lb (4.6-kg) spayed female domestic shorthaired cat was presented to the Louisiana State University School of Veterinary Medicine Veterinary Teaching Hospital for evaluation of painful periocular swelling of both eyes of about one month's duration.
HISTORY
The cat was kept indoors but was allowed to go outside. The cat was current on vaccinations and had no travel history outside of Louisiana. The results of feline leukemia virus and feline immunodeficiency virus testing performed before referral were negative.

Vital Stats
Previous therapies used to treat the swelling included administering an injectable long-acting corticosteroid, a topical triple antibiotic, and oral clindamycin. After an initial improvement in clinical signs, the ocular signs quickly returned and were unresponsive to oral cefadroxil therapy.
EXAMINATIONS
On physical examination, the cat's temperature, pulse, respiratory rate, and body condition score were normal.
An ophthalmic examination revealed periocular soft tissue swelling, epiphora, and exophthalmia with decreased retropulsion of both eyes. These findings were most pronounced in the left eye (Figure 1). A lack of menace response in the left eye was noted along with a markedly reduced palpebral reflex, which had resulted in significant central exposure keratitis and the development of a superficial corneal ulcer.

1. A 4-year-old cat evaluated for painful periocular swelling in both eyes. Note the marked periocular tissue swelling present in the left eye. Epiphora and elevated third eyelids are present in both eyes. Central corneal changes are evident in the left eye and correspond to the area of exposure keratitis secondary to lagophthalmos.
No active ocular motility could be elicited from the globe, and lateral strabismus was noted. There was a marked amount of conjunctival thickening and hyperemia of the left eye. Moderate conjunctival hyperemia and chemosis were noted in the right eye. Intraocular pressures measured by applanation tonometry (Tono-Pen XL—Reichert Technologies) were 19 mm Hg for the right eye and 35 mm Hg for the left eye. Pupillary light reflexes were slow and incomplete in the left eye and were normal in the right eye.
On slit-lamp examination, diffuse corneal edema and keratic precipitates were noted in both eyes. Additionally, marked aqueous flare was noted bilaterally along with pars planitis in the right eye and rubeosis iridis and posterior synechia in both eyes. Pigment deposition and inflammatory changes affecting the anterior lens capsule were noted bilaterally. An inferior bullous retinal detachment was noted in the right eye. Fundic examination of the left eye was limited because of the anterior segment changes.
DIFFERENTIAL DIAGNOSES
Differential diagnoses for bilateral ocular and orbital disease in this case included infectious causes such as systemic fungal disease (cryptococcosis, aspergillosis, blastomycosis, penicilliosis, histoplasmosis)1-9 or aerobic or anaerobic bacteria,10,11 neoplastic processes (lymphosarcoma, squamous cell carcinoma, osteoma, osteosarcoma, fibrosarcoma),10,12,13 and primary inflammatory disorders (eosinophilic, pseudotumor).11,14,15
DIAGNOSTIC TESTS
Because of the patient's fractious nature, the cat was placed under general anesthesia and intubated to allow maintenance of anesthesia with isoflurane while a complete blood count (CBC), a serum chemistry profile, thoracic radiography, and orbital and ocular ultrasonography and aspiration were performed. A temporary tarsorrhaphy of the left eye was also performed to provide corneal protection.
CBC and serum chemistry profile
The only significant abnormalities noted were hyperproteinemia (8.2 g/dl; reference range = 6 to 7.5 g/dl) and a mild mature neutrophilia (15.4 x 103/µl; reference range = 2.5 to 12.5 x 103/µl), which were both attributed to inflammation.
Thoracic radiography
Thoracic radiography showed a pneumomediastinum with extension into the retroperitoneum, likely induced by barotrauma. Barotrauma most commonly occurs as a complication of mechanical ventilation and results in extra-alveolar air accumulation.
On follow-up radiography, no pulmonary parenchymal abnormalities were found, the pneumomediastinum had resolved, and thoracic radiography results were considered normal.
Ultrasonography
Ocular ultrasonography confirmed a partial retinal detachment in the right eye. A diffusely thickened and completely detached retina was identified in the left eye (Figure 2).

2. A dorsal oblique plane ultrasonographic image of the left globe showing a diffusely thickened and completely detached retina.
Orbital ultrasonography results showed a homogenous retrobulbar mass, measuring 2.2 x 1.5 cm, deforming the posterior sclera on the left side (Figure 3). A similar but smaller (1.9 x 0.8 cm) homogenous mass was noted in the right orbit. Fine-needle aspiration of the left retrobulbar mass was performed for cytologic examination.

3. A dorsal plane ultrasonographic image of the homogenous left retrobulbar mass displacing the sclera.
Cytology
Moderate numbers of adequately preserved nucleated cells with mild-to-moderate blood contamination were noted (Figure 4). Moderate numbers of small, mature lymphocytes; a few slightly vacuolated macrophages; and a few nondegenerate neutrophils were present. Low numbers of small (2 or 3 µm long and 1 or 2 µm wide), round-to-oval yeast were present both extracellularly and phagocytosed by the macrophages. These yeast were surrounded by a thin clear halo and contained a small, eccentrically located, crescent-shaped purple nucleus.
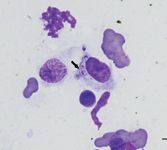
4. Cytologic examination findings from the fine-needle aspiration of the left retrobulbar mass seen in Figure 3. Note the macrophage with phagocytosed Histoplasma capsulatum yeast; rare, small, mature lymphocytes; and aggregates of erythrocytes (Diff-Quik-Dade Behring; bar = 20 µm).
The cytologic interpretation was granulomatous inflammation with intracellular Histoplasma capsulatum organisms.
DEFINITIVE DIAGNOSIS
Based on the results of the examinations and diagnostic tests, panuveitis, secondary glaucoma, retinal detachment, and retrobulbar granuloma of both eyes secondary to systemic histoplasmosis were diagnosed.
TREATMENT AND PATIENT OUTCOME
Antifungal therapy with itraconazole was initiated at 5 mg/kg given orally twice a day, and the topical carbonic anhydrase inhibitor dorzolamide was initiated three times a day to control the intraocular pressure in both eyes. Additionally, the eyes were treated with the topical nonsteroidal anti-inflammatory diclofenac three times a day. The left eye was treated with topical ciprofloxacin three times a day to prevent infection of the corneal ulcer. Clinical signs were found to gradually improve over the following four weeks.
Unfortunately, owner compliance in this case was poor, and a relapse of clinical signs occurred after the owner discontinued medical therapy several months later. On subsequent examination, the patient had developed right forelimb lameness and joint effusion. Radiography of the forelimb showed lytic bony changes of the distal humerus and proximal radius and ulna. Histoplasma capsulatum organisms were identified by cytologic examination of aspirated joint fluid. Ultimately, because of the severity of changes in the left eye, enucleation was recommended and performed by the referring veterinarian. Antifungal therapy was reinstituted, and the patient continues to be monitored.
DISCUSSION
Histoplasmosis is a systemic mycotic infection caused by H. capsulatum, a dimorphic, saprophytic fungus that prefers nitrogen-rich soil and a humid environment.5,6 Geographic distribution is primarily reported for temperate and subtropical regions. In the United States, cases are most commonly reported in regions of the Ohio, Missouri, and Mississippi river valleys.7-9 Histoplasmosis is often diagnosed between January and April, presumably because of the increased moisture in the soil during this time.16 Although an uncommon disorder, histoplasmosis is the second most common fungal infection reported in cats.16
Typical histoplasmosis is the result of inhaling fungal spores (microconidia) that originate from the mycelial phase of the fungus. At body temperature, these spores convert to yeast and are subsequently phagocytized by pulmonary macrophages.7,17 The organism undergoes intracellular replication in reticuloendothelial cells and may then become disseminated throughout the body through lymphatic and hematogenous routes.9,18 This dissemination results in clinical disease that can affect the lungs, liver, spleen, choroid, lymph nodes, intestinal mucosa, bone marrow, adrenal glands, bones, and skin, producing a variety of clinical signs.7,9
Clinical signs and ocular findings
In most cases, cats with the disseminated form of histoplasmosis have a nonspecific constellation of signs including weight loss, weakness, dehydration, depression, fever, anorexia, and anemia.16,18-21 The incidence of respiratory signs (dyspnea, tachypnea, coughing) ranges from 39% to 45%.16,20
Ocular abnormalities were reported in 24% of cases in one study.16 The most common ocular abnormalities in patients with disseminated histoplasmosis included granulomatous chorioretinitis, anterior uveitis, and retinal detachment.6,9 In one retrospective study in which 20 cats with histoplasmosis received an ophthalmic examination, retinal detachments were noted in 25%.20 Granulomatous blepharitis and optic neuritis have also been reported.17,19 To our knowledge, this case is the first with bilateral retrobulbar granulomas secondary to systemic histoplasmosis.
Diagnosis
Diagnosing this condition can be challenging since serologic tests for H. capsulatum antigen often yield false negative results in patients with active disease.7,19 Thus, identification of the organism on cytologic preparations is the most likely way to obtain a rapid definitive diagnosis.5
Although ocular aspiration was not performed in this case to confirm the organisms within the eye, it has been reported that in cats with systemic mycoses, intraocular inflammation is caused by the organism within the eye and not as a result of a systemic inflammatory response.9
Recently, urine antigen testing (MVista—MiraVista Diagnostics) has become an important tool in the diagnosis of histoplasmosis. The sensitivity of this test has been reported as 94% for the detection of antigen in the urine of affected cats.22
Treatment
The highest reported success rate for the treatment of histoplasmosis has been with itraconazole (5 mg/kg orally twice a day).21,23 However, the administration of a combination of amphotericin B and ketoconazole has also been successful.19 Systemic antifungal agents should be administered until clinical signs resolve. Protracted therapy is often required.
Monitoring serial antigen concentrations will help you evaluate a patient's response to therapy and determine for how long the therapy should be continued.24 In one study, only 55% of cats survived to discharge; the median duration of treatment for these cats was five months.20
It can be difficult to clear infectious organisms from within the eye, and the eye may serve as a future nidus of infection even after protracted systemic antifungal therapy. Cases with ocular involvement are considered to have disseminated disease, which is associated with a poor-to-guarded prognosis.
Nonspecific therapy for secondary ocular signs is also necessary. Topical anti-inflammatory agents are aggressively given to reduce anterior uveitis. Topical corticosteroids (1% prednisolone acetate, 0.1% dexamethasone) may be administered in cats without corneal ulceration. For cats with corneal ulceration, administering a topical nonsteroidal anti-inflammatory agent, such as 0.03% flurbiprofen or 0.1% diclofenac, until the corneal ulcer is resolved is recommended. Topical anti-inflammatory agents are not effective for treating posterior uveitis, so when not contraindicated, a systemic anti-inflammatory agent should also be administered.
Administering a topical cycloplegic (e.g. 1% atropine) is also recommended to reduce ocular pain and the incidence of posterior synechiae; however, this drug is contraindicated in patients with secondary glaucoma. In this case, intraocular pressure values were elevated in the left eye and within established reference ranges in the right eye.25 However, given the degree of uveitis seen on examination, intraocular pressure values were considered inappropriate, and therapy with a topical carbonic anhydrase inhibitor (2% dorzolamide) was instituted three times daily in both eyes.
CONCLUSION
Consider systemic fungal infections in cats with systemic illness, especially when ocular findings are present. Ophthalmic examination results can help you diagnose systemic mycosis as there is often involvement of the uveal tract.9 Ongoing evaluation of ocular involvement is an important component in managing cats with systemic mycosis.
Renee T. Carter, DVM, DACVO*
Melissa Kubai, DVM**
J. Daniel Rodriguez, MVZ Esp, DACVR***
Department of Veterinary Clinical Sciences
School of Veterinary Medicine
Louisiana State University
Baton Rouge, LA 70803
Aradhana Gupta, DVM, MVSc, DACVP†
Angela B. Royal, DVM, MS, DACVP††
Department of Pathobiological Sciences
School of Veterinary Medicine
Louisiana State University
Baton Rouge, LA 70803
*Dr. Carter's current address is Baton Rouge Veterinary Specialists, 3803 S. Sherwood Forest Blvd., Baton Rouge, LA 70816.
* *Dr. Kubai's current address is the Department of Veterinary Clinical Medicine, College of Veterinary Medicine, University of Illinois, Urbana, IL 61802.
* * *Dr. Rodriguez's current address is Bahia de Espíritu Santo #43 Int Fuego 405, Col. Anahuac, Del Miguel Hidalgo, Mexico, DF C.P 11320.
†Dr. Gupta's current address is the Department of Clinical Pathology, College of Veterinary Medicine, Kansas State University, Manhattan, KS 66506.
† †Dr. Royal's current address is the Veterinary Medical Diagnostic Laboratory, College of Veterinary Medicine, University of Missouri, 900 E. Campus Drive, Columbia, MO 65211.
REFERENCES
1. Wilkinson GT. Feline cryptococcosis: a review and seven case reports. J Small Anim Pract 1979;200:749-768.
2. Hamilton HL, Whitley RD, McLaughlin SA. Exophthalmos secondary to aspergillosis in a cat. J Am Anim Hosp Assoc 2000;36:343-347.
3. Wilkinson GT, Sutton RH, Grono LR. Aspergillus spp. infection associated with orbital cellulitis and sinusitis in a cat. J Small Anim Pract 1982;23:127-131.
4. Peiffer RL, Belkin PV, Janke BH. Orbital cellulitis, sinusitis, and pneumonitis caused by penicillium sp in a cat. J Am Vet Med Assoc 1980;176:449-451.
5. Johnson LR, Fry MM, Anez KL, et al. Histoplasmosis infection in two cats from California. J Am Anim Hosp Assoc 2004;40:165-169.
6. Mahaffey E, Gabbert N, Johnson D, et al. Disseminated histoplasmosis in three cats. J Am Anim Hosp Assoc 1977;13:46-51.
7. Wolf AM, Belden MN. Feline histoplasmosis: a literature review and retrospective study of 20 new cases. J Am Anim Hosp Assoc 1984;20:995-998.
8. Percy DH. Feline histoplasmosis with ocular involvement. Vet Pathol 1981;18:163-169.
9. Gionfriddo JR. Feline systemic fungal infections. Vet Clin North Am Small Animal Pract 2000;30:1029-1050.
10. Stiles J, Townsend WM. Feline ophthalmology. In: Gelatt KN, ed. Veterinary ophthalmology. 4th ed. Ames, Iowa: Blackwell, 2007;1095-1164.
11. van der Woerdt A. Orbital inflammatory disease and pseudotumor in dogs and cats. Vet Clin North Am Small Animal Pract 2008;38:389-401.
12. Cottrill NB, Carter JD, Pechman RD, et al. Bilateral orbital parosteal osteoma in a cat. J Am Anim Hosp Assoc 1987;23:405-408.
13. Gilger BC, McLaughlin SA, Whitley RD, et al. Orbital neoplasms in cats: 21 cases (1974-1990). J Am Vet Med Assoc 1992;201:1083-1086.
14. Dziezyc J, Barton CL. Exophthalmia in a cat caused by an eosinophilic infiltrate. Prog Vet Comp Ophthalmol 1992;2:91-93.
15. Billson FM, Miller-Michau T, Mould JR, et al. Idiopathic sclerosing orbital pseudotumor in seven cats. Vet Ophthalmol 2006;9:45-51.
16. Davies C, Troy GC. Deep mycotic infections in cats. J Am Anim Hosp Assoc 1996;32:380-391.
17. Peiffer RL, Belkin PV. Ocular manifestations of disseminated histoplasmosis in a cat. Feline Pract 1979;9:24-29.
18. Clinkenbeard KD, Wold AM, Cowell RL, et al. Feline disseminated histoplasmosis. Comp Vet Med Pract Vet 1989;11:1223-1235.
19. Bromel C, Greene CE. Histoplasmosis. In: Green CE, ed. Infectious diseases of the dog and cat. 4th ed. St. Louis, Mo: Elsevier Saunders, 2012;614-621.
20. Aulakh HK, Aulakh KS, Troy GC. Feline histoplasmosis: a retrospective study of 22 cases (1986–2009). J Am Anim Hosp Assoc 2012;48:182-187.
21. Lin Blache J, Ryan K, Arceneaux K. Histoplasmosis. Compend Contin Educ Vet 2011;33:E1-E11.
22. Cook AK, Cunningham LY, Cowell AK, et al. Clinical evaluation of urine Histoplasma capsulatum antigen measurement in cats with suspected disseminated histoplasmosis. J Feline Med Surg 2012;14:512–515.
23. Hodges RD, Legendre AM, Adams LG, et al. Itraconazole for the treatment of histoplasmosis in cats. J Vet Intern Med 1994;8:409-413.
24. Garcia J. Lecture link: new trends in handling histoplasmosis. Vet Med 2012;107:396.
25. Miller PE, Pickett JP, Majors LJ, et al. Evaluation of two applanation tonometers in cats. Am J Vet Res 1991;52:1917-1921.