Clinical Exposures: Copper-associated hepatitis in a Doberman pinscher
The outcome in this dog was not good, illustrating the necessity of identifying this disorder early.
A 6-year-old spayed female Doberman pinscher was presented for an annual wellness examination. The dog weighed 68 lb (31 kg), which was 15 lb less than it weighed at its last visit five months before. The owner reported that the dog had been less interested in food for the past few weeks but was still eating. The owner also noted that the dog was exhibiting polyuria and polydipsia.

Figure 1. A lateral abdominal radiograph of the dog in this case showing cranial displacement of the gastric axis and loss of serosal detail.
PHYSICAL EXAMINATION AND LABORATORY FINDINGS
The results of a physical examination were unremarkable. The dog's body condition score was 3/5.
The complete blood count results were unremarkable. The relevant results of the serum chemistry profile are presented in Table 1.
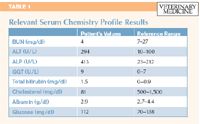
Table 1: Relevant Serum Chemistry Profile Results
DIAGNOSIS
Liver dysfunction was suspected based on these findings. The differential diagnoses included chronic hepatitis, neoplasia, chronic hepatopathy, and toxicosis.
A radiographic examination was performed, and the thoracic radiographs were unremarkable. The abdominal radiographs revealed cranial displacement of the gastric axis and loss of serosal detail, suggestive of microhepatia and ascites, respectively (Figure 1). An abdominal ultrasonographic examination showed a small, hypoechoic, heterogeneous, and irregularly marginated liver. A small amount of free peritoneal fluid was seen throughout the abdomen, which was consistent with ascites.
The radiographic and ultrasonographic changes associated with the liver indicated severe chronic liver disease, but other diffuse disease processes such as neoplasia could not be ruled out.
The owners elected euthanasia. Postmortem liver histologic changes were compatible with severe, chronic-active portal hepatitis, with strong positive results on staining for copper with rhodamine stain. The diagnosis was copper-associated chronic hepatitis.
DISCUSSION
Chronic hepatitis in Doberman pinschers, also known as Doberman hepatitis, is a disorder associated with histologic features of chronic active hepatitis, cholestasis, and cirrhosis. The disease is usually diagnosed in middle-aged spayed female dogs.1 The high incidence of chronic hepatitis in Doberman pinschers compared with some other breeds suggests the disease is hereditary.1-3
The pathogenesis of chronic hepatitis in Doberman pinschers has been debated for several years; the disease may be immune-mediated.1-3 Most affected dogs have chronic hepatitis and high liver copper concentrations, but the role of the high copper concentration is unclear.1-3 Whether the increased copper concentration is the result of concurrent cholestasis or whether the liver disease is a result of copper toxicosis is yet to be determined.4 Hepatic copper accumulation can result from increased uptake, a primary defect in hepatic copper metabolism, or altered biliary copper excretion.2,3
Copper-associated hepatitis is well-described in other breeds, such as Bedlington terriers,5 Labrador retrievers,6 and Dalmatians.7 The average canine copper liver concentration is 200 to 400 ppm per dry weight liver. Copper concentrations in breeds with primary copper storage disease vary between 600 to above 2,200 ppm.1
Affected Dobermans can start accumulating copper at the age of few months, but the clinical signs usually develop between 4 and 7 years of age.1 The signs are usually nonspecific and result from liver dysfunction.2,3 The initial clinical signs are usually subtle and intermittent and can begin as a calmer demeanor and loss of appetite.1,2 Gradually, the signs become more evident and can include salivation, nausea, and intermittent vomiting.1 In advanced stages, polyuria, polydipsia, icterus, diarrhea, ascites, and signs of hepatic encephalopathy may also be present. The progression of the clinical signs is variable but usually occurs over months.
Diagnostic findings
The first and most consistent laboratory abnormality reported in Bedlington terriers with copper-associated hepatitis is elevated alanine transaminase (ALT) activity.1,5 In Doberman pinschers, the first sign can be elevated ALT activity in a young (1 to 3 years) usually female dog.1 Other laboratory findings include elevations in other liver enzyme activities (alkaline phosphatase and gamma-glutamyl transferase) or evidence of loss of liver functions (decreased BUN, cholesterol, albumin, or glucose concentrations).
Radiographic findings are usually nonspecific, such as microhepatia and ascites.1 An ultrasonographic examination is helpful in ruling out other liver diseases.1 The liver size is usually normal but can be decreased if the disease has progressed to cirrhosis. The liver echogenicity is either normal, increased, decreased, or irregular.1
The only method for definitive diagnosis is histologic examination of a liver biopsy sample. Findings are consistent with chronic active hepatitis, cholestasis, and cirrhosis in later stages. The earliest changes are infiltration by inflammatory cells (macrophages, lymphocytes and plasma cells) and collagen deposition (scar tissue formation). These changes begin around the small hepatic vein branches. Progression of the disease leads to further fibrosis, inflammation, and hepatocyte loss beginning among zone 3 hepatocytes around the terminal hepatic vein branches.8
The copper concentrations in liver tissue can be assessed quantitatively or by spectrophotometric methods.1 The limitation of the quantitative methods is that a large amount of tissue is required. Alternatively, histochemical stains can be used for semiquantitative assessment, which may give a subjective result.2
Treatment options
Common treatments for copper-associated hepatitis include chelation with penicillamine or trientine, administration of zinc, antioxidant supplementation, and dietary modification. Penicillamine mobilizes copper from tissues and promotes copper excretion in urine. It also has anti-inflammatory, immunosuppressive, and antifibrotic effects and may increase the synthesis of metallothionein (a copper-binding protein). Penicillamine is administered at a dosage of 10 to 15 mg/kg b.i.d. orally.9 This drug should not be given with any other medications or supplements and is potentially teratogenic, so inform owners about safe handling practices.
Copper chelator therapy with penicillamine in subclinical dogs can normalize the copper concentrations and reverse histologic damage.10 One study showed that in dogs treated with D-penicillamine, copper retention was effectively reduced and the histologic appearance of hepatic lesions improved.4
Trientine hydrochloride (10 to 15 mg/kg orally b.i.d.)9 is used when penicillamine is not tolerated. This drug can also have a teratogenic effect in animals, so owners should be informed about safe handling practices.
Zinc (100 mg orally divided b.i.d.)9 orally reduces copper absorption from the diet by inducing metallothionein production by the intestinal mucosal cells. The removal of hepatic copper resulting from zinc administration is relatively slow, so it should not be used as sole therapy and can be used as maintenance treatment. In people, it has been used as first-line therapy in asymptomatic patients.
Diet changes should be made to reduce the absorption of copper from the intestinal tract.1,6 Foods that contain a high amount of copper include eggs, liver, shellfish, organ meats, beans, mushrooms, chocolate, nuts, and cereals and should be avoided.1 Commercial diets low in copper are available (e.g. Veterinary Diet canine HEPATIC LS—ROYAL CANIN; Prescription Diet l/d Canine Hepatic Health—Hill's Pet Nutrition). A study in Labrador retrievers demonstrated that a low-copper diet can stabilize the liver copper concentration in the high normal range.6 The dogs in the study were not at the clinical stage of the disease, so it has not been determined whether dietary management improves the clinical signs.
Since chronic inflammatory liver diseases and cholestatic liver diseases result in reduced protection against oxidative stress, the use of antioxidants could be helpful.3,5 Common antioxidants used in animals with liver diseases are S-adenosylmethionine (SAMe) (20 mg/kg orally once a day), milk thistle (20 to 50 mg/kg orally once a day), and N-acetylcysteine (70 mg/kg orally t.i.d.),11 which help replenish glutathione, and certain vitamins such as vitamin E.
Unfortunately, the prognosis for dogs with cirrhosis or decompensated liver function at presentation is poor,12-14 and once clinical signs of chronic hepatitis in Dobermans are seen, the response to treatment is poor. Diagnosing and managing the disease in the early stages results in a better prognosis. Early detection, by regularly measuring ALT activity in dog breeds at risk of developing copper-associated hepatitis, can help identify patients that would benefit from early intervention. The exact cause of chronic hepatitis is still unclear, and clinical trials are still necessary for understanding the best treatment approach.
Michal O. Hess, DVM
50 Greenway N
Forest Hills, NY 11375
REFERENCES
1. Hoffmann G, Rothuizen J. Copper-associated chronic hepatitis. In: Bonagura JD, Twedt DC, eds. Kirk's current veterinary therapy XIV: Small animal practice. St. Louis, Mo: Saunders Elsevier, 2009;557-561.
2. Mandigers PJ, van den Ingh TS, Bode P, et al. Association between liver copper concentration and subclinical hepatitis in Doberman pinschers. J Vet Intern Med 2004;18(5):647-650.
3. Spee B, Mandigers PJ, Arends B, et al. Differential expression of copper-associated and oxidative stress related proteins in a new variant of copper toxicosis in Doberman pinschers. Comp Hepatol 2005;4(1):3.
4. Spee B, Arends B, van den Ingh TS, et al. Copper metabolism and oxidative stress in chronic inflammatory and cholestatic liver diseases in dogs. J Vet Intern Med 2006;20(5):1085-1092.
5. Teske E, Brinkhuis BG, Bode P, et al. Cytological detection of copper for the diagnosis of inherited copper toxicosis in Bedlington terriers. Vet Rec 1992;131(2):30-32.
6. Hoffmann G, Jones PG, Biourge V, et al. Dietary management of hepatic copper accumulation in Labrador retrievers. J Vet Intern Med 2009;23(5):957-963.
7. Webb CB, Twedt DC, Meyer DJ. Copper-associated liver disease in Dalmatians: a review of 10 Dogs (1998-2001). J Vet Intern Med 2002;16(6):665-668.
8. Thornburg LP. Histomorphological and immunohistochemical studies of chronic active hepatitis in Doberman Pinschers. Vet Pathol 1998;35(5):380-385.
9. Willard M. Canine hepatic diseases, including chronic hepatitis: more confusing than we first thought, in Proceedings. Western Vet Conf, 2010.
10. Mandingers PJ, van den Ingh TS, Bode P, et al. Improvement in liver pathology after 4 months of D-penicillamine in 5 doberman pinschers with subclinical hepatitis. J Vet Intern Med 2005;19(1):40-43.
11. Twedt DC. Treatment of liver disease: medical and nutritional management, in Proceedings. Western Vet Conf, 2010.
12. Sevelius E. Diagnosis and prognosis of chronic hepatitis and cirrhosis in dogs. J Small Anim Pract 1995;36(12):521-528.
13. Watson PJ, Chronic hepatitis in dogs: a review of current understending of the aeteiology, progression and treatment. Vet J 2004;167(3):228-241.
14. Poldervaart JH, Favier RP, Penning LC, et al. Primary hepatitis in dogs: a retrospective review (2002-2006). J Vet Intern Med 2008;23(1):72-80.