Clinical Exposures: Why it's important to examine the entire radiographic image
A 2-year-old intact male Boston terrier was evaluated because of a recent onset of gagging and vomiting.
A 2-year-old intact male Boston terrier was evaluated because of a recent onset of gagging and vomiting. Physical examination showed no abnormalities, and the owners declined laboratory testing. Abdominal radiography was performed.
RADIOGRAPHIC FINDINGS
On the lateral view, two roughly parallel soft-tissue opacity lines with distinct margins in the caudodorsal thorax were noted (Figure 1A). On the ventrodorsal view, two diverging soft-tissue opacity lines extended cranially from the lateral aspects of T12 to the cardiac silhouette (Figure 1B). These lines represented the caudal esophagus distended with gas.
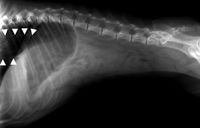
Figure 1A. Lateral and ventrodorsal abdominal radiographs of a Boston terrier that was evaluated because of gagging and vomiting. Soft-tissue opacity lines represent the caudal esophagus distended with gas (arrows).
On both views, the gastric axis was deviated cranially, consistent with a small liver. The stomach was moderately distended with gas; no ingesta was present. There was no radiographic evidence of intestinal distention, a foreign body, or a mass. The patient was thin, as indicated by the "tucked-up" appearance of the abdomen. This resulted in decreased radiographic abdominal detail.

Figure 1B Lateral and ventrodorsal abdominal radiographs of a Boston terrier that was evaluated because of gagging and vomiting. Soft-tissue opacity lines represent the caudal esophagus distended with gas (arrows).
RADIOGRAPHIC CONCLUSIONS
The radiographic diagnoses included caudal megaesophagus, a small liver, and aerophagia. No evidence of gastrointestinal obstruction was noted.
No radiographic signs indicated the cause of the megaesophagus. Possible causes included sedation or anesthesia, a caudal esophageal foreign body, esophagitis from vomiting due to pancreatitis, idiopathic or congenital conditions, heavy metal toxicosis, Addison's disease, polymyositis, polyneuritis, and myasthenia gravis. Most often, no inciting cause of megaesophagus is determined.
The dog's small liver may have been due to hepatic insufficiency (e.g. cirrhosis, portosystemic shunt), or it may be normal in a deep-chested dog such as this one. Additional diagnostic tests, such as those noted below, would have been necessary to rule out hepatic insufficiency.
The gas distention of the stomach was secondary to aerophagia.
ADDITIONAL DIAGNOSTIC RECOMMENDATIONS
When megaesophagus is noted on abdominal radiographs, such as in this case, thoracic radiographs obtained without patient sedation are indicated to verify persistent, diffuse esophageal enlargement, as well as to evaluate for aspiration pneumonia. It is possible that some of the dog's gagging reported by the owners may have been coughing. In all cases of megaesophagus, it is extremely important to evaluate for aspiration pneumonia, as it is a common and serious complication.
A three-view, thoracic radiographic study is recommended because focal pneumonia may be masked by recumbent atelectasis in the dependent lobes. An esophagram may be of benefit to evaluate esophageal motility as well as to evaluate for evidence of esophagitis, a caudal esophageal foreign body, stricture, or neoplasia. Barium liquid may be administered orally first to outline the esophagus or a foreign body and to evaluate the mucosal surface. Subsequently, feeding the animal a mixture of barium and food helps evaluate the lumen size, determine whether a stricture is present, and evaluate motility. This step is unnecessary (and may increase the risk of aspiration) if poor esophageal motility and a large-diameter lumen are verified on the images obtained after administration of liquid barium.
Ideally, fluoroscopy is used for real-time evaluation of esophageal function; however, fluoroscopy is not commonly available, and plain radiographs still provide a good deal of information.
Diagnostic tests to investigate the cause of the small liver would include measuring preprandial and postprandial serum bile acid concentrations; a serum chemistry profile including blood urea nitrogen, bilirubin, and total protein concentrations and liver enzyme activities; and abdominal ultrasonography. If laboratory findings suggest a portosystemic shunt but one is not found with ultrasonography, further diagnostic tests should include operative mesenteric portography, computed tomography portography, and scintigraphy.
Unfortunately in this case, additional information is not available because the owner did not present the dog to the primary veterinarian for follow-up evaluation.
DISCUSSION
This case is an excellent example of the importance of evaluating the entire radiographic image. In this case, the cause of the gagging and presumed vomiting was found not in the abdomen, where the study was focused, but in the thorax on the edges of the radiographic views.
Other examples of significant findings that are located in an area different from the usual focus of radiographs include pulmonary metastatic nodules on the edge of an abdominal study and a lytic lesion on a proximal humerus seen on a thoracic study.
Developing a systematic method for reading radiographs can help veterinarians avoid missing a lesion. This process is much like the systematic approach to the physical examination. My method of reading abdominal radiographs is to first evaluate nonabdominal structures such as the thorax, ribs, spine, pelvis, hindlimbs (if included), and peripheral soft tissues. Then I evaluate the overall abdominal contrast followed by an examination of specific structures. I move in a cranial-to-caudal direction—diaphragm, liver, gastrointestinal tract, spleen, kidneys and retroperitoneal area, urinary bladder, and sublumbar region. The particular method you use is unimportant, as long as a methodology is in place and used consistently. Some people like to read radiographs right to left, cranial to caudal, top of the film to the bottom, or periphery to center by organ or organ system.

Figure 2A. The same radiographs as in Figures 1A & 1B with the contrast and brightness adjusted to make the caudal esophagus more apparent.
When evaluating radiographic films of the abdomen, a bright light source (hot light) should be used to evaluate any anatomic areas that are overexposed. Overexposure of thoracic structures routinely occurs with abdominal radiographic technique.

Figure 2B. The same radiographs as in Figures 1A & 1B with the contrast and brightness adjusted to make the caudal esophagus more apparent.
If the images are made by using a digital radiography system, it also is important to adjust the brightness and contrast as needed, so all parts of the image can be fully evaluated. One of the advantages of using digital radiography is the ability to adjust contrast and brightness during image interpretation (Figures 2A & 2B).
Editors' note: The American Association of Veterinary Radiologists offers interactive radiology rounds online every other week. To learn more, visit aavr.org.
Julie Ekedahl, VMD, DACVR, Veterinary Imaging Specialists of Idaho, Boise, ID 83702, provided this case report.