CVC Highlight: How I assess postsurgical pain in cats
Dr. Mark Epstein gives his thoughts on feline pain management.
Cats have historically been a difficult species in which to assess pain. Since pain is a multidimensional experience (encompassing both physical and emotional components), an observer must be astute to pick up signs of moderate or mild pain in cats. These signs may be exhibited not only by the onset of new behaviors, but also by the absence of usual behaviors. A few tools are available to help practitioners score pain in cats postoperatively.

Mark E. Epstein, DVM, DABVP, DAAPM
THE SUBTLE SIGNS OF PAIN
Cats in severe postoperative pain may become aggressive, tearing at their bandages or acting frantic and vocalizing (Table 1). However, some cats lie very still or may even purr when they are distressed or in pain.
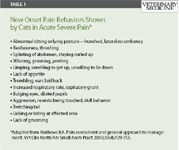
Table 1
In addition, cats exhibit many of the signs that dogs do when they are in pain, but they are more likely to become extremely ill-tempered and may twitch their tails as a sign of agitation and remain in a crouched, hunched position. Also, cats may be unwilling to use the litter box and are more likely than dogs to exhibit withdrawn behavior such as hiding in the back of the cage. Some research attempting to correlate facial expressions in cats to their level of pain is currently under way.

Tek Image/GettyImages
PAIN SCALES
A standardized self-rating pain scale is routinely used in human medicine, and a validated acute pain scale (the Glasgow Composite Measure Pain Scale) is available in dogs.1,2 No validated acute pain scale exists for cats (although the Glasgow group is working on one at this time), but one pain scoring tool in common use is the Colorado State University Pain Scale. (Download a PDF of this pain scale at http://www.ivapm.org/attachments/097_CSU%20Acute%20Pain%20Scale%20-%20Feline%20v.2.pdf.)
AN APPROACH TO PAIN SCORING
Our hospital uses a hybrid of a numeric rating scale that is dynamic and interactive. The patient's pain is scored on a 0 to 10 scale—0 being no pain and 10 being the worst possible pain that might be expected for that specific procedure. Taking the type of procedure performed into consideration has improved pain scoring predictability,3,4 since the worst possible pain for an ovariohysterectomy (for example) will be much different (less) than the worst possible pain for limb amputation. The technique uses
1. Observation of the patient before any interaction
2. Observation of the patient while interacting
3. Palpation of the painful site.
This technique uses the totality of the observer's experience and patient's signs to render the score. It is important that, whenever possible, the same individual—one familiar with the patient's personality before the surgery—score the patient throughout the entire postoperative period to diminish interobserver variation.
For example, a patient that has undergone a 2-cm laceration repair and, three hours postoperatively, is guarding the surgery site and flinches when it is palpated may receive a score of 6/10. This is an unusual amount of pain given the relatively minimal tissue damage and inflammation and the fact that, with a local block, one could realistically expect the site to be completely pain-free (numb with a pain score of 0/10). But a cat that has undergone a fracture repair and, 12 hours postoperatively, is 60% weightbearing and withdraws slightly when the limb is palpated but yet exhibits few other signs of discomfort might receive only a 4/10 since this procedure involves significant trauma and inflammation and there is no expectation that the patient will be 100% weightbearing or pain-free. However, both of these patients might benefit by added pain management intervention.
A prime issue, of course, may not be the actual number (i.e. whether it is 2/10 vs. 3/10), but rather the trend in the number as the observer (usually a technician) monitors over time. If the pain score appears to be increasing, additional intervention would be warranted, and after intervention, the pain score should decrease.
It is important to note that this scoring system is not scientifically validated and it is not linear (i.e. a score of 6/10 is not necessarily twice as painful as a 3/10). However, it is an easy, rapid adaptation of basic behavior-based principles described by a number of authors.
SYSTOLIC HYPERTENSION AS AN INDICATOR
It is worth mentioning that systolic hypertension in cats may be the only physiologic parameter shown to correlate with postoperative pain in animals. In one study, cats receiving no (or inadequate) dosages of butorphanol (0.1 mg/kg) after ovariohysterectomy often had increased systolic blood pressure and serum cortisol concentrations when compared with cats receiving adequate pain medication.5 The cats with increased systolic blood pressure also demonstrated behavioral changes associated with pain (withdrawal, remaining still, and vocalizing when moved), while cats that had lower blood pressure were willing to move and returned to a normal personality sooner. However, stress in addition to pain may also lead to systemic hypertension, and the practicality of using systolic blood pressure as a gauge of pain has not been determined.
FINAL THOUGHTS
By using a standardized proposed pain scale and attempting to eliminate score variations, we can strive to alleviate suffering in our feline patients by quickly recognizing clinical signs of pain and taking appropriate pain control measures.
Mark E. Epstein, DVM, DABVP (canine and feline), DAAPM
Carolinas Animal Pain Management
TotalBond Veterinary Hospital Forestbrook
3200 Union Road
Gastonia, NC 28056
REFERENCES
1. Holton L, Reid J, Scott EM, et al. Development of a behaviour-based scale to measure acute pain in dogs. Vet Rec 2001;148(17):525-531.
2. Morton CM, Reid J, Scott EM, et al. Application of a scaling model to establish and validate an interval level pain scale for assessment of acute pain in dogs. Am J Vet Res 2005;66(12):2154-2166.
3. Holton LL, Scott EM, Nolan AM, et al. Comparison of three methods used for assessment of pain in dogs. J Am Vet Med Assoc 1998;212(1):61-66.
4. Lascelles BD, Cripps PJ, Jones A, et al. Efficacy and kinetics of carprofen, administered preoperatively or postoperatively,for the prevention of pain in dogs undergoing ovariohysterectomy. Vet Surg 1998;27(6):568-582.
5. Smith JD, Allen SW, Quandt JE, et al. Indicators of postoperative pain in cats and correlation with clinical criteria. Am J Vet Res 1996;57(11):1674-1678.