Diagnostic imaging for linear foreign bodies in cats
Linear foreign bodies are a well-recognized problem in small-animal practice.
Linear foreign bodies are a well-recognized problem in small-animal practice. In cats, the most common linear foreign bodies are string, carpet, and plastic.1 Clinical signs of a foreign body include vomiting, regurgitation, ptyalism, inappetence, anorexia, depression, diarrhea, abdominal pain, and dehydration. Early diagnosis helps prevent complications such as peritonitis due to gastric or intestinal perforation.2
Since the clinical signs are nonspecific, imaging is almost always necessary to diagnose linear foreign bodies. In our teaching hospital, we use several imaging techniques including survey abdominal radiography, upper gastrointestinal (GI) series with barium or iodinated contrast material, survey or contrast abdominal compression radiography, and abdominal ultrasonography. The advantages and disadvantages of these techniques are discussed below, including a case report in which three of these imaging studies were used to definitively diagnose a linear foreign body in a cat.
CASE REPORT
A 1-year-old spayed female domestic longhaired cat was presented to the Veterinary Teaching Hospital at Kansas State University with a 24-hour history of coughing, vomiting, polydipsia, anorexia, lethargy, and abdominal pain.
Examinations and diagnostic tests
On physical examination, the cat appeared depressed and had dry, tacky mucous membranes. The cat's abdomen was tense on palpation. Oral examination findings were unremarkable. Based on the history and physical examination results, the differential diagnoses included a GI foreign body, pancreatitis, and gastroenteritis of unknown cause.
A complete blood count revealed polycythemia (packed cell volume = 60%; reference range = 30% to 45%), increased plasma protein (9.1 g/dl; reference range = 6 to 8 g/dl), leukopenia (total white blood cell count = 3,600/μl; reference range = 5,500 to 19,500/μl) with slight neutropenia (2,400/μl; reference range = 2,500 to 12,500/μl), and marked lymphopenia (800/μl; reference range = 2,000 to 7,000/μl). These results were consistent with dehydration and inflammation. Intravenous fluid therapy with a crystalloid solution was given to correct dehydration.
Survey radiography
Abnormal findings on ventrodorsal and right lateral survey abdominal radiographs were a plicated small intestine, fluid opacity within the pylorus, and a heterogeneous mix of gas and soft tissue opacity in the fundic region of the stomach (Figures 1A & 1B). A left lateral view was also obtained to complete the evaluation of the stomach and pylorus. All views revealed normal serosal detail.
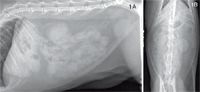
1A &1B. Right lateral and ventrodorsal abdominal radiographs of the cat in this report showing plication of the small intestines and fluid opacity within the pylorus.
Survey compression radiography
Because this case allowed an additional opportunity for instructing students, abdominal compression radiography with a compression paddle applied gently and uniformly to the left ventrolateral abdomen was performed to isolate the small intestine and enhance the visibility of its shape and contour. This view demonstrated bunching of the small intestine and plication without gas segmentation of the intestine (Figure 2).

2. A right lateral abdominal compression radiograph of the cat in this report showing the plicated small intestine.
Because plication was identified on the survey and abdominal compression radiographs, a positive contrast GI study was not necessary. We have included right lateral and ventrodorsal views from a different case as an example of a contrast study in a cat with a linear foreign body (Figures 3A & 3B).

3A & 3B. Right lateral and ventrodorsal barium contrast abdominal radiographs showing a linear foreign body outline throughout the intestine in a cat from a different case.
Ultrasonography
For teaching purposes, an ultrasonographic evaluation was also performed. Ultrasonography helps to evaluate the length and location of the linear foreign body (as evidenced by intestinal plication), degree of peristalsis, and stomach and intestinal wall integrity and thickness. It also helps to rule out free peritoneal fluid, which is an early indicator of bowel perforation and peritonitis. Linear echogenic material and plication were noted within the duodenum extending into the proximal jejunum (Figures 4A & 4B). The stomach and intestinal walls were a normal thickness. Fluid and peristalsis were present in the stomach and duodenum, which are normal findings. An ultrasonogram of normal small intestine is shown for comparison (Figure 5). Because the linear foreign body extended to the jejunum, endoscopic removal was not an option.

4A. An ultrasonogram of the cat in this report demonstrating the characteristic appearance of plication in the small intestine.

4B. Small intestinal plication produced by a linear foreign body (arrows) in the cat in this report.
Treatment
The cat was anesthetized and prepared for surgery, and an exploratory laparotomy was performed. A linear foreign body was palpated in the stomach and extended from the duodenum to the colon (Figure 6). A gastrotomy and two enterotomies were needed to access and remove a cotton string. No complications occurred during surgery or recovery. The cat continued to receive fluid therapy, antibiotics, and analgesics for three days and was discharged with instructions for the owner to feed a bland diet.
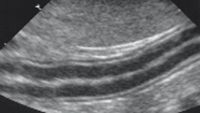
5. An ultrasonogram of a normal small intestine in a cat. Note the smooth and normal shape of the small intestine. The intestinal walls are easily identified.
DISCUSSION
Practitioners must know the indications for and advantages and disadvantages of different imaging techniques as well as be able to identify the typical abnormalities consistent with linear foreign bodies that are seen with these techniques.

6. An intraoperative picture of the cat in this report showing the plicated small intestine.
Survey abdominal radiography
Survey abdominal radiography is always recommended in vomiting patients. In our hospital, ventrodorsal and right lateral views are standard. The advantages of abdominal radiography are that it is noninvasive, provides immediate results, and is relatively inexpensive and readily available. The disadvantages include radiation exposure and summation or superimposition of soft tissues over the stomach and intestines.3
On survey radiographs, intestinal linear foreign bodies can cause abnormal shape, contour, and luminal content pattern.2,4 They can also produce an accordion-like pleating, shortening, or gathering of the small intestine because of peristalsis.1-6 Because the antimesenteric border of the intestine is longer than the mesenteric border, gas commonly becomes trapped in pockets formed by the pleats, resulting in an abnormal pattern of unconnected round, tapered, and short tubular gas shapes. Repositioning the patient in the opposite lateral recumbency causes redistribution of intestinal gas, which serves as negative contrast media for this second lateral view. This negative contrast can be helpful in localizing the foreign body.7-9 That is particularly true in the case of pyloric foreign bodies because in right lateral recumbency, gas accumulates in the fundus, but in left lateral recumbency, gas is present in the pyloric region.9,10 On the right and left lateral views, evaluating gas within the small or large intestine may help differentiate various segments of the intestine as well as elucidate abnormalities.9 Additional abnormalities such as free air, loss of serosal detail (denoting abdominal effusion), and soft tissue masses are easily observed on survey films.2,4
Compression radiography
Compression radiography is a fast and easy way to isolate and evaluate abdominal structures, including the small intestine.11 This technique's advantage is the isolation of organs of interest to provide evaluation without summation and superimposition from other organs.11,12
The technique is simple and has been described elsewhere.11 Briefly, the area of the target organ of interest is compressed with a wooden or plastic spoon, paddles, or any rigid and radiolucent material that has a surface 1.5 times the size of the area of interest. Minimize patient discomfort by compressing the area with your hand before placing the radiolucent device over it, and then slip your hand out.11 Compression can also be used with a contrast study.
In this case, the compression technique elucidated an area of small-bowel plication. To prevent potential complications such as bowel rupture and peritonitis, carefully consider that friable intestine may be present when you perform compression in patients with severe abdominal pain. We have used abdominal compression radiography in several cases with no complications; however, we recommend compressing the abdomen gently.
Positive contrast upper GI radiography
Another technique that can be used to diagnose linear foreign bodies is a positive contrast upper GI study, but it was unnecessary in this case. These studies can be used to evaluate small intestinal foreign bodies, strictures, mucosal disease, and abnormal transit times.1,4,10
A GI study can be done with either micropulverized barium sulfate solution or water-soluble iodinated products. Barium sulfate suspensions are radiopaque, provide excellent mucosal detail, and are inexpensive.13,14 If leakage into the peritoneal cavity occurs, barium combined with enteric contents may cause granulomas or adhesions.4 By comparison, iodinated ionic solutions have a rapid transit time, are nonirritating to serosal surfaces, are rapidly resorbed following extraluminal leakage, and can be followed quickly by endoscopic evaluation if indicated.15 However, iodinated ionic solutions are hypertonic, which cause an influx of fluid into the GI tract, making them contraindicated in debilitated and dehydrated patients.4,15 Thus, although vomiting has been reported within 15 to 30 minutes after administration of undiluted iohexol (a nonionic iodinated positive contrast agent) in experimental studies in cats, we recommend nonionic contrast media.16
Contrast studies are time-consuming. In some cases, further attempts to define the specific site and type of obstruction with contrast media may only delay and complicate surgery or further compromise the patient.4
Ultrasonography
Ultrasonography has become increasingly important in diagnosing GI disease.17,18 Ultrasonographic studies are noninvasive, accurate for diagnosing linear foreign bodies, and provide information relative to GI function and disease location.19,20 Abnormal echogenic material within the lumen indicates a foreign body2; however, the appearance of foreign material will vary depending on its physical properties. Linear foreign bodies are linear structures located eccentrically within the lumen of thickened, plicated bowel.19 The integrity of the intestinal wall can be evaluated based on the presence of fluid or air outside the GI tract. In the absence of free gas, a combination of ultrasonographic findings such as bright mesenteric fat, peritoneal effusion, fluid-filled stomach and intestines, wall thickening, reduced motility, and loss of wall layering (the mucosa, submucosa, muscle, and serosa are usually easily seen with ultrasonography as adjacent layers) may be associated with perforation.21 In this case, the presence of linear echogenic material within the stomach and extending into the small intestine, with associated plication, was recognized as linear foreign material without evidence of GI perforation.
CONCLUSION
All abdominal radiographic views, including right lateral, left lateral, and ventrodorsal, are important in identifying foreign material in the gi tract. The main goal of placing patients in these different positions is to use intestinal gas as negative contrast to localize the foreign body. It is important to distinguish the normal location of air and fluid in every view. When an isolated organ evaluation is needed, compression radiography is an inexpensive and easy technique. Positive contrast studies provide useful information regarding the location and the degree of the obstruction and should be used in small-animal practice. Ultrasonographic evaluation provides information about the shape and position of the stomach or bowel and the presence of intraluminal structures, as well as the ability to measure bowel wall thickness and evaluate intestinal wall layers. Typical intestinal shapes associated with linear foreign bodies, intussusceptions, and other kinds of foreign materials have been described elsewhere. 1
Using the most accurate, least invasive diagnostic imaging technique is imperative for optimizing care in patients with linear foreign bodies. Additional studies are indicated when the diagnosis is uncertain with survey radiography. It will not be necessary to perform all of these techniques in every patient.
Luis M. Gonzalez, DVM, MS*
David S. Biller, DVM, DACVR
Laura J. Armbrust, DVM, DACVR
Department of Clinical Sciences
College of Veterinary Medicine
Kansas State University
Manhattan, KS 66506
*Dr. Gonzalez's current address is Department of Small Animal Clinical Sciences, Virginia-Maryland Regional College of Veterinary Medicine, Virginia Polytechnic Institute and State University, Blacksburg, VA 24061.
REFERENCES
1. Bebchuk TN. Feline gastrointestinal foreign bodies. Vet Clin North Am Small Anim Pract 2002;32:861-880.
2. Burk RL, Ackerman N. The abdomen. In: Small animal radiology and ultrasonography: a diagnostic atlas and text. 2nd ed. Philadelphia, Pa: WB Saunders Co, 1996;215-426.
3. Bowlus RA, Biller DS, Ambrust LJ, et al. Clinical utility of pneumogastrography in dogs. J Am Anim Hosp Assoc 2005;41:171-178.
4. Riedesel EA. The small bowel. In: Thrall DE, ed. Textbook of veterinary diagnostic radiology. Philadelphia, Pa: WB Saunders Co, 2002;639-660.
5. Ljunggren G. The radiological diagnosis of some acute abdominal disorders in the dog. J Am Vet Radiol Soc 1964;5:5-14.
6. Root CR, Lord PF. Linear radiolucent gastrointestinal foreign bodies in cats and dogs: their radiographic appearance. J Am Vet Radiol Soc 1971;12:45-53.
7. Farrow CS. Radiographic characterization of gastric foreign material in a dog. Mod Vet Pract 1986;67:716-718.
8. Ticer JW. The abdomen. In: Ticer JW, ed. Radiographic technique in veterinary practice. 2nd ed. Philadelphia, Pa: WB Saunders Co, 1984;312-325.
9. Armbrust LJ, Biller DS, Hoskinson JJ. Case examples demonstrating the clinical utility of obtaining both right and left lateral abdominal radiographs in small animals. J Am Anim Hosp Assoc 2000;36:531-536.
10. Root CR. Interpretation of abdominal survey radiographs. Vet Clin North Am 1974;4:763-803.
11. Armbrust LJ, Biller DS, Hoskinson JJ. Compression radiography: An old technique revisited. J Am Anim Hosp Assoc 2000;36:537-541.
12. Farrow CS. Abdominal compression radiography in the dog and cat. J Am Anim Hosp Assoc 1978;14:337-342.
13. Carrig CB, Mostosky UV. The use of compression in abdominal radiography of the dog and cat. J Am Anim Hosp Assoc 1976;17:178-181.
14. Mahaffey MB, Barber DL. The stomach. In: Thrall DE, ed. Textbook of veterinary diagnostic radiology. 4th ed. Philadelphia, Pa: WB Saunders Co, 2002;615-638.
15. Wallack ST. Handbook of veterinary contrast radiography. Solana Beach, Calif: San Diego Veterinary Imaging Inc, 2003;1-27.
16. Williams J, Biller D, Miyabayashi T, et al. Evaluation of iohexol as a gastrointestinal contrast medium in normal cats. Vet Radiol Ultrasound 1993;34:310.
17. Moon ML, Biller DS, Armbrust LJ. Ultrasonographic appearance and etiology of corrugated small intestine. Vet Radiol Ultrasound 2003;44:199-203.
18. Lamb CR. Recent developments in diagnostic imaging of the gastrointestinal tract of the dog and cat. Vet Clin North Am Small Anim Pract 1999;29:307-342.
19. Tidwell AS, Penninck DG. Ultrasonography of gastrointestinal foreign bodies. Vet Radiol Ultrasound 1992;33:160-169.
20. Tyrrell D, Beck C. Survey of the use of radiography vs. ultrasonography in the investigation of gastrointestinal foreign bodies in small animals. Vet Radiol Ultrasound 2006;47:404-408.
21. Boysen SR, Tidwell AS, Penninck DG. Ultrasonographic findings in dogs and cats with gastrointestinal perforation. Vet Radiol Ultrasound 2003;44:556-564.