Guidelines for evaluating hypercalcemic cats
Review the steps to evaluating a hypercalcemic cat.
Calcium plays an essential role in numerous biochemical pathways, and adequate amounts are required for optimal cell growth, neuromuscular function, blood coagulation, and cell membrane stability. Consequently, the serum concentration of ionized (active) calcium is tightly controlled through complex interplay among parathyroid hormone (PTH), calcitonin, and vitamin D metabolites. In healthy individuals, calcium absorption from the intestinal tract, calcium release from bone, and calcium conservation or excretion by the kidneys are all carefully regulated to optimize ionized calcium (iCa) concentrations.

Illustration by Paul Petersen
Hypercalcemia is a fairly uncommon disorder in cats, but it can cause substantial patient morbidity and is associated with serious medical disorders such as neoplasia and renal failure.1 In this article, I review the definition of hypercalcemia and the steps to take when clinically evaluating a hypercalcemic cat.

ESSENTIAL ELEMENTS
DEFINING AND CONFIRMING HYPERCALCEMIA
Circulating calcium exists in three distinct forms: bound to serum proteins (40%); complexed with citrate, phosphate, and other anions (8%); or ionized (52%).2 The ionized fraction is the biologically active form, and an elevated iCa concentration defines true hypercalcemia. The calcium reported on standard serum chemistry profiles is a total calcium value (tCa; i.e. bound, complexed, and ionized), so changes in acid-base status and serum protein concentrations frequently affect this result.
In dogs, the effect of serum proteins may be mitigated by calculating the corrected or adjusted total calcium value. This formula has not been validated in cats and should not be used.3 Instead, measure serum iCa concentrations in cats with elevated tCa concentrations, with tCa concentrations at the upper end of the normal range, or exhibiting risk factors associated with hypercalcemia (e.g. calcium oxalate urolithiasis, chronic renal failure).2 Several commercially available in-house machines can accurately measure iCa concentrations, or a reference laboratory may be used. Samples must be collected anaerobically, handled correctly, and shipped appropriately, as changes in pH can substantially alter the percentage of calcium bound to protein and, thus, the iCa concentration.
Total calcium concentrations can be spuriously elevated. Lipemia and hemolysis can affect colorimetric measurements. Before considering additional diagnostic tests, always verify hypercalcemia, either by repeating a tCa measurement in a fasted patient or by determining the iCa concentration.
SIGNS OF HYPERCALCEMIA
Cats appear to be more resistant to the clinical consequences of hypercalcemia than are dogs, and it is not unusual to document substantial hypercalcemia in an apparently normal patient.2 The most prevalent clinical signs reported in hypercalcemic cats are vague and nonspecific, such as lethargy, depression, and anorexia.2 Other changes include an increase in thirst and urination due to antidiuretic hormone antagonism at the renal collecting ducts, or dysuria and abdominal pain secondary to calcium-containing uroliths (Table 1).
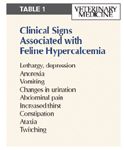
Table 1
As serum calcium concentrations continue to rise, gastrointestinal disturbances (vomiting and constipation) or neuromuscular dysfunction (twitching and seizures) may be noted. If the serum calcium-phosphorus product exceeds 70, tissue mineralization and secondary organ damage—primarily renal—are expected. Precipitous increases in serum calcium concentrations are often fatal.2
CAUSES OF HYPERCALCEMIA
In general, hypercalcemia reflects increased gastrointestinal uptake or increased calcium release from bone; decreased renal calcium excretion is rarely the cause. Mnemonics have been devised to help you remember all the causes of hypercalcemia. For example, Table 2 is a modification of the GOSH DARN IT list.
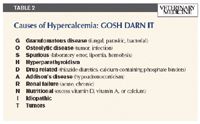
Table 2
The most comprehensive recent case series of feline hypercalcemia was published in 2000.1 This retrospective study evaluated 71 cats and defined hypercalcemia on the basis of tCa concentrations > 11 mg/dl (reference range = 9.2 to 10.2 mg/dl). The authors reported that the most common disorders identified were neoplasia (n = 21), renal failure (n = 18), urolithiasis (n = 11), and primary hyperparathyroidism (n = 4). However, iCa concentrations were not measured, so some of these may not have been true feline hypercalcemia cases. In fact, many cats with chronic kidney disease have normal iCa concentrations and, thus, are not truly hypercalcemic.4
Cats with neoplasia had higher serum calcium concentrations (13.5 ± 2.5 mg/dl) than cats with renal failure did (11.5 ± 0.5 mg/dl).1 Eight of the 11 cats with urolithiasis had calcium oxalate stones confirmed at surgery.1 An underlying cause of hypercalcemia was not identified in any of the cats with urolithiasis. Based on the exclusion of other recognized causes, these patients fit the criteria for idiopathic hypercalcemia.5 This term was first proposed in the late 1990s and is now applied to any cat with unexplained, repeatable hypercalcemia. Since it is a diagnosis of exclusion, every reasonable effort must be made to rule out other likely causes.

Table 3
The SHIRT list (Table 3) is a mnemonic devised to help you remember the common causes of feline hypercalcemia. Table 4 summarizes the classic serum chemistry profile findings in cats with the commonly identified causes of hypercalcemia and demonstrates the parameters expected in idiopathic cases.

Table 4
APPROACH TO THE HYPERCALCEMIC PATIENT
In cases of mild (tCa < 13 mg/dl) and moderate (tCa = 13 to 15 mg/dl) hypercalcemia, therapy can be delayed while the diagnosis is pursued in a logical, stepwise fashion.2 In severely hypercalcemic patients (tCa > 15 mg/dl) or those with a serum calcium-phosphorus product > 70, immediate intervention to lower serum calcium concentrations may be necessary.6 In such cases, it is imperative to establish a diagnosis quickly, and it is appropriate to investigate all likely causes simultaneously.

Table 5
In many cases, a database that includes a complete history, a physical examination, retroviral testing, a complete blood count, a serum chemistry profile, a urinalysis, thoracic and abdominal radiographic examinations, and an abdominal ultrasonographic examination will establish a preliminary diagnosis. In other cases, specific evaluation of calcium homeostasis may be necessary (Table 5). The following is a brief review of the standard diagnostic tests, and an algorithm (Figure 1) is also presented as a guide.

Figure 1
1. Physical examination
Since neoplasia is the most likely cause of moderate to severe hypercalcemia, a thorough physical examination is essential, paying particular attention to the mammary glands, peripheral lymph nodes, and skin. Abdominal palpation may reveal organomegaly, or thoracic auscultation may point toward pulmonary, mediastinal, or pleural disease. Examine the cervical region carefully, as parathyroid adenomas are sometimes palpable.7
2. Retroviral testing
ELISA tests for feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) infections are appropriate in any cat whose retroviral status is uncertain. Always verify a positive ELISA test result with an alternative test, such as an immunofluorescent antibody (IFA) test. Vaccination against FIV infection will result in positive results with ELISA, IFA, and Western blot tests for as long as vaccine antibodies persist.
If a hypercalcemic cat is FeLV positive, the index of suspicion for lymphoma is higher. FIV infection does not necessarily increase the incidence of neoplasia, but it may predispose patients to osteolytic or granulomatous disease.
3. Complete blood count
Anemia suggests chronic inflammatory disease, renal compromise, or myeloinfiltrative disorders. Cats with idiopathic hypercalcemia or hyperparathyroidism are not anemic, so finding a low hematocrit suggests occult cancer or organ dysfunction. Carefully evaluate the leukogram for abnormal cell distribution or morphology, which indicates lymphoma or leukemia.
4. Serum chemistry profile
Since hypercalcemia is both a cause and consequence of renal failure, markers of kidney function (blood urea nitrogen [BUN] and creatinine concentrations) are of particular interest. In general, only severe hypercalcemia is thought to cause renal injury; mild hypercalcemia in an azotemic patient is more likely to be secondary to kidney disease. It is important to measure iCa concentrations in azotemic cats before starting a complex work-up, as elevations in tCa concentrations without increases in iCa concentrations are common in this population.4
Serum phosphorus concentrations often indicate the cause of hypercalcemia. Hyperphosphatemia suggests intrinsic renal failure, vitamin D toxicosis, or osteolytic disease. In contrast, serum phosphorus is generally subnormal in cats with hyperparathyroidism, which may explain the low incidence of renal compromise reported in these individuals.8
In addition, the serum chemistry profile may indicate liver disease (increased liver enzyme activities, hyperbilirubinemia) or gastrointestinal tract dysfunction (hypoalbuminemia or hypocholesterolemia). Investigate any abnormalities.
5. Thyroxine (T4) concentration
Measure serum T4 concentration in any patient more than 7 years old or in any cat showing signs of hyperthyroidism. A total T4 concentration is generally sufficient, but equivocal results can be investigated with free T4 measurement. Cats with hyperthyroidism often have increased PTH concentrations. This elevation may be an appropriate physiologic response to increased calciuresis, but it can certainly confuse patient evaluation.9 Hypercalcemia (based on tCa concentration) was reported in two hyperthyroid cats, but no direct association was demonstrated and no information was provided about reversibility.1
6. Urinalysis
Although profound polydipsia is not commonly noted in cats with hypercalcemia, urine concentration may be lower than expected (specific gravity < 1.040). Isosthenuria may indicate intrinsic renal failure, but it has been noted in cats with severe hypercalcemia for many reasons.
Perform a urine sediment examination in all cats with hypercalcemia. Calcium oxalate urolithiasis is commonly noted in hypercalcemic cats, and morbidity may occur from urinary tract obstruction and infection.5,10,11
7. Thoracic radiography
A three-view thoracic radiographic examination (right and left lateral plus ventrodorsal or dorsoventral) is appropriate since both primary and metastatic neoplasia may cause hypercalcemia. Pay particular attention to the mediastinal region, and scrutinize all bony structures for lytic lesions.
8. Abdominal radiography
Although soft tissue changes are more easily identified with ultrasonography than with abdominal radiography, you can readily identify calculi in the kidneys, ureters, or the urinary bladder by using abdominal radiography. In addition, distinctive lytic bony lesions may be noted in the vertebrae of cats with multiple myeloma.
9. Abdominal ultrasonography
A scan to look for organomegaly, lymphadenopathy, bladder tumors, or other masses is a logical part of the hypercalcemic work-up. Any lesions should be aspirated or biopsied.
As calcium oxalate uroliths are commonly noted in hypercalcemic cats, pay close attention to the renal pelves and ureters.10,11 If you have any concerns about ureteral obstruction, an abdominal radiographic examination may assist with calculi detection.
10. PTH concentration
Serum PTH concentrations will be low in cats with neoplasia, vitamin D-related toxicosis, or osteolytic disease. Although elevated PTH concentrations are the hallmark of primary hyperparathyroidism, PTH concentrations must be interpreted in conjunction with iCa concentrations.8 In cats with appropriate feedback mechanisms, elevated iCa concentrations suppress PTH release. Consequently, high normal PTH concentrations are inappropriate in patients with elevated iCa concentrations. Cats with renal failure have variable PTH concentrations, but iCa concentrations are generally normal. Patients with idiopathic hypercalcemia are expected to have low normal PTH concentrations.
11. PTH-related protein concentration
Many tissues synthesize a protein with marked similarities to endogenous PTH. This protein is called parathyroid hormone-related protein (PTH-rP), and it binds with PTH receptors in bone and kidney. In normal animals, PTH-rP concentrations are essentially undetectable, but one of the mechanisms for paraneoplastic hypercalcemia is the release of PTH-rP by malignant tissues.12
In dogs, PTH-rP production has also been documented in association with inflammatory disorders, but that is not the case in cats.13 Although PTH-rP is not a highly sensitive marker for cancer in cats, it is regarded as specific. Consequently, an elevated concentration strongly suggests malignancy. Various types of carcinoma (e.g. squamous cell, bronchogenic, renal, thyroid) and lymphoma are most often associated with PTH-rP secretion in cats.2,12
12. Vitamin D concentration
Vitamin D metabolism is complex, as dietary sources require hepatic and renal activation to become metabolically active. Elevated serum vitamin D concentrations indicate excessive dietary supplementation or accidental ingestion of a cholecalciferol rodenticide. However, the standard vitamin D assay only measures 25-hydroxycholecalciferol; some potent vitamin D products (e.g. calcipotriene, present in psoriasis cream; calcitriol, commonly used in cats with renal failure) are not detected. If vitamin D toxicosis is suspected but not substantiated by test results, carefully question owners. Also consider granulomatous diseases, as a high serum calcitriol concentration was documented in a cat with atypical mycobacterium infection and secondary hypercalcemia.14
Depending on the dose ingested, vitamin D toxicosis can cause profound hypercalcemia and hyperphosphatemia, with progressive and refractory acute renal failure.
Audrey K. Cook, BVM&S, MRCVS, DACVIM, DECVIM-CA
Department of Small Animal Clinical Sciences
College of Veterinary Medicine
Texas A&M University
College Station, TX 77843
REFERENCES
1. Savary KC, Price GS, Vaden SL. Hypercalcemia in cats: a retrospective study of 71 cases (1991-1997). J Vet Intern Med 2000;14(2):184-189.
2. Schenck PA, Chew DJ, Behrend EN. Update on hypercalcemic disorders. In: August J. Consultations in feline internal medicine. 5th ed. St. Louis, Mo: Elsevier, 2005;157-168.
3. Flanders JA, Scarlett JM, Blue JT, et al. Adjustment of total serum calcium concentration for binding to albumin and protein in cats: 291 cases (1986-1987). J Am Vet Med Assoc 1989;194(11):1609-1611.
4. Barber PJ, Elliott J. Feline chronic renal failure: calcium homeostasis in 80 cases diagnosed between 1992 and 1995. J Small Anim Pract 1998;39(3):108-116.
5. Midkiff AM, Chew DJ, Randolph JF, et al. Idiopathic hypercalcemia in cats. J Vet Intern Med 2000;14(6):619-626.
6. Wallace MS. Endocrine emergencies, in Proceedings. Atlantic Coast Vet Conf 2001.
7. Kallet AJ, Richter KP, Feldman EC, et al. Primary hyperparathyroidism in cats: seven cases (1984-1989). J Am Vet Med Assoc 1991;199(12):1767-1771.
8. Barber PJ. Disorders of the parathyroid glands. J Feline Med Surg 2004;6(4):259-269.
9. Barber PJ, Elliot J. Study of calcium homeostasis in feline hyperthyroidism. J Small Anim Pract 1996;37(12):575-582.
10. McClain HM, Barsanti JA, Bartges JW. Hypercalcemia and calcium oxalate urolithiasis in cats: a report of five cases. J Am Anim Hosp Assoc 1999;35(4):297-301.
11. Kyles AE, Hardie EM, Wooden BG, et al. Clinical, clinicopathologic, radiographic, and ultrasonographic abnormalities in cats with ureteral calculi: 163 cases (1984-2002). J Am Vet Med Assoc 2005;226(6):932-936.
12. Bolliger AP, Graham PA, Richard V, et al. Detection of parathyroid hormone-related protein in cats with humoral hypercalcemia of malignancy. Vet Clin Pathol 2002;31(1):3-8.
13. Fradkin JM, Braniecki AM, Craig TM, et al. Elevated parathyroid hormone-related protein and hypercalcemia in two dogs with schistosomiasis. J Am Anim Hosp Assoc 2001;37(4):349-355.
14. Mealey KL, Willard MD, Nagode LA, et al. Hypercalcemia associated with granulomatous disease in a cat. J Am Vet Med Assoc 1999;215(7):959-962.