Local and regional anesthesia techniques, Part 1: Overview and five simple techniques
Add these 5 techniques to your clinical toolbox to help lessen your patients' pain.
Local and regional anesthesia techniques in veterinary practice have many advantages. These techniques

Illustration by Elaine Kurie
- Provide effective preemptive and multimodal analgesia
- Reduce the amount of inhalational agent needed to maintain anesthesia, resulting in improved cardiopulmonary stability during anesthesia
- Modulate the sympathetically driven stress response to surgical trauma
- Reduce the development of central sensitization.
Multimodal analgesia can be provided with combinations of local anesthetics, opioids, and alpha2 agonists.
In this article, we give an overview of drugs used for local and regional anesthesia and then discuss five anesthetic techniques—infiltration anesthesia, splash blocks, digital nerve blocks, intravenous regional anesthesia, and soaker-type catheters. We will discuss additional techniques—intra-articular stifle blocks, brachial plexus nerve blocks, intercostal nerve blocks, intrapleural nerve blocks, maxillary and mandibular nerve blocks, and epidural anesthesia and analgesia—in subsequent articles throughout this year. All of these techniques are easy to perform, do not require special equipment, and can greatly enhance the analgesic management of veterinary patients.
DRUGS USED FOR LOCAL AND REGIONAL ANALGESIA AND ANESTHESIA
Three general drug groups are used to produce regional anesthesia and analgesia in veterinary patients—local anesthetics, opioids, and alpha2 agonists.
Local anesthetic drugs
Local anesthetics are weak bases that are poorly soluble in water. Commercially available preparations are formulated as acidic hydrochloride salts to improve stability and water solubility. The pH of commercial preparations of local anesthetics ranges from 3.9 to 6.6. Most local anesthetics are marketed as racemic mixtures of left and right enantiomers. The enantiomers vary in pharmacokinetic, pharmacodynamic, and toxic properties.1,2
TABLE 1: Characteristics of Amide-linked and Ester-linked Local Anesthetics
Structure and effects. Local anesthetic molecules consist of a lipophilic unsaturated aromatic ring and hydrophilic portion, usually a tertiary amine, separated by a connecting hydrocarbon chain. The lipophilic portion is essential for the anesthetic activity. Local anesthetics are categorized as amino esters or amino amides based on the chemical bond between the aromatic ring and the hydrocarbon chain of the molecule (Table 1). Although lidocaine (known as lignocaine in the United Kingdom) and bupivacaine are most commonly used in small-animal practice, a variety of local anesthetics are available, varying in their chemical structures, potency, onset of action, and duration of effect (Table 2).1,2
Local anesthetics block nerve conduction in all types of neurons, including all pain (A delta and C fibers), sensory, motor, proprioceptive, and sympathetic nerve fibers (Table 3). The minimum concentration of local anesthetic necessary to block conduction is higher for motor nerve fibers than for sensory fibers, so sensory anesthesia can occur without muscle blockade. Typically, autonomic preganglionic B fibers are blocked first. A delta and C sensory fibers are blocked before and at lower concentrations than larger sensory A beta, motor A alpha, and proprioceptive A gamma fibers. The order of blockade varies with anatomical location, the specific nerve, and the local anesthetic used.1,2
TABLE 2: Local Anesthetics and Their Physical, Chemical, and Pharmacodynamic Properties
The active form of local anesthetics, the nonionized base, diffuses across the axonal nerve membrane where it blocks the generation and conduction of nerve impulses by inhibiting voltage-gated sodium channels. The degree of drug ionization depends on the local anesthetic's dissociation constant (pKa) and the surrounding tissue's pH. When the pKa and pH are identical, 50% of the drug is ionized and 50% is nonionized. The dissociation constants of local anesthetics vary from 7.6 to 9.1, which means that less than 50% of local anesthetic exists in the active, nonionized form at the normal tissue pH of 7.4. The potency, speed of onset of nerve blockade, and duration of anesthesia are related to the degree of ionization of the local anesthetic molecule and, thus, lipid solubility. Alkalizing the local anesthetic by adding sodium bicarbonate increases the percentage that exists in the nonionized, lipid-soluble form and also reduces pain on injection. Thus, buffering the local anesthetic solution with sodium bicarbonate before administration may increase efficacy as well as decrease pain on injection. Acidosis at the injection site, as occurs with tissue infection, increases the ionized portion of the drug, decreasing the local anesthetic's efficacy.1,2
TABLE 3: Types of Neurons Blocked with Local Anesthetics
Systemic uptake. Local anesthetics are rapidly absorbed across mucosal, pleural, and peritoneal surfaces, with high bioavailability. Absorption from epidural and subcutaneous sites is slower, with lower bioavailability. The ultimate plasma concentration is determined by the rate of systemic uptake and the rate of drug clearance. The systemic absorption of a local anesthetic is determined by the dose administered (volume and concentration), the drug's protein binding and lipid solubility, the injection site's vascularity, and the use of a vasoconstrictor. Higher doses and increased injection site vascularity will increase systemic absorption.
All local anesthetics cause vasodilation, which makes systemic drug absorption more rapid. Epinephrine can be added to cause vasoconstriction and slow systemic absorption, increasing the intensity and the duration of blockade and reducing the potential for toxicity. In addition, epinephrine may have some local anesthetic effects itself.1 The usual concentration of epinephrine is 5 µg/ml, or 1:200,000. This concentration can be obtained by adding 0.1 ml of 1:1,000 (0.1 mg) epinephrine to 20 ml of the local anesthetic. Some commercially available local anesthetics already contain epinephrine. Epinephrine can cause tissue necrosis along wound edges and, rarely, ventricular dysrhythmias. Never use epinephrine to block distal extremities, including digits, ears, or tails, because of the potential for local tissue ischemia.1-3

TABLE 4:Indications and Drug Dosages for Local and Regional Anesthesia Techniques
Toxicity. Local anesthetics can cause severe toxic reactions after unintentional intravenous administration, vascular absorption of an excessive dose, or ingestion of topical local anesthetic preparations. Intravenous injection of bupivacaine is highly toxic to the cardiovascular system and central nervous system, resulting in agitation, muscular twitching, seizures, unconsciousness, coma, respiratory arrest, cardiac depression, dysrhythmias, hypotension, and death. Always aspirate the syringe before injecting any local anesthetic to avoid intravenous or intra-arterial injection.
Base dosage calculations on lean body weight, and always calculate the maximum safe dose to avoid toxicosis (Table 2). Animals with hepatic impairment or reduced hepatic blood flow (hypotension, cardiac failure), geriatric patients, and neonates are more prone to develop toxicosis with amide-linked local anesthetics, so reduce doses by 40% to 60%. In addition, cats should receive lower doses than dogs do since they are more likely to develop signs of toxicosis because they metabolize local anesthetics more slowly and, to a lesser extent, because of their decreased ability for glucuronidation.1-3
Relative or absolute overdosage of local anesthetics results in agitation, muscular twitching, seizures, unconsciousness, coma, respiratory arrest, cardiac depression, dysrhythmias, hypotension, and death.1,2 Some effects may be masked by general anesthesia, and dysrhythmias, hypotension, and respiratory arrest may be the only observable signs of toxicosis. Allergic reactions can occur but are uncommon. Benzocaine and prilocaine, and less commonly procaine and lidocaine, have been associated with the development of methemoglobinemia in dogs and cats.2 Cats are at increased risk for developing methemoglobinemia and Heinz-body anemia with benzocaine-containing products, including Cetacaine (a combination of benzocaine, butamben, and tetracaine), so these products should be avoided in cats.2
When given in high volumes epidurally or spinally, local anesthetics can cause excessive blockade of sympathetic neurons, resulting in hypotension, and excessive blockade of motor neurons, resulting in paralysis of intercostal muscles and the diaphragm.1,2
Opioids
Opioids are sometimes added to local anesthetics to increase efficacy and extend the duration of the block. The efficacy of peripherally injected opioids is likely due to a combination of factors, including direct effects on opioid receptors in the periphery, anti-inflammatory effects, systemic absorption, and action at the spinal cord due to slow retrograde axonal transport along the nerve.4-6
Directly applying opioids to a peripheral nerve at high concentrations can produce analgesia that is not naloxone-reversible and is thought to be a nonspecific local anesthetic-like action.4 In addition, opioid mu and kappa receptors are present on the distant peripheral terminals of C fibers, and these receptors increase in number and become activated when there is inflammation at the site.4-6 Opioids attenuate the excitability of peripheral nociceptive terminals of primary afferent neurons during inflammation by inhibiting high-voltage activated calcium channels, which decreases the propagation of action potentials and the release of C fiber excitatory transmitters, such as substance P.4-6
Opioids may also mediate local analgesia through anti-inflammatory effects. Opioid receptors on immune cells and endogenous opioid peptides expressed in resident immune cells within peripheral inflamed tissue mediate lymphocyte function suppression and cytokine synthesis and release. Both mu and kappa opioid agonists have shown potent anti-inflammatory activity.5,6
Morphine is often used in intra-articular and epidural blocks, along with local anesthetics, and seems to provide additional analgesia in people and dogs.7-9 Buprenorphine has been shown to extend the duration of analgesia with brachial plexus and epidural blocks in people, compared with local anesthetic administration alone.10-13 Epidural morphine and buprenorphine have induced thermal nociception in cats, but morphine antinociception lasted longer and was more intense.14 The mechanism for the increased efficacy and duration of analgesia with peripherally administered opioids appears to be related to the lipophilicity of the opioid since the highly lipophilic buprenorphine provided a longer duration of satisfactory analgesia in people after a brachial plexus block than did the less lipophilic sufentanil.13 The anti-inflammatory effects of opioids likely also play a role in prolonging analgesia.5 Minimal adverse affects are associated with the peripheral administration of opioids because doses administered peripherally result in low plasma concentrations in most species.2,5
Alpha2 agonists
Alpha2 agonists, such as medetomidine, can be added to local anesthetic blocks to extend the duration and increase the efficacy of the block.15-18 Alpha2 agonists likely exert these effects through several mechanisms, including vasoconstriction, resulting in decreased systemic absorption of local anesthetics; facilitation of C fiber blockade by the local anesthetic; and action at the spinal cord due to slow retrograde axonal transport along the nerve.17 Norepinephrine is a principal neurotransmitter in the sympathetic nervous system that is also involved in nociception through alpha2-adrenergic receptors expressed on peripheral sensory neurons. In pathological pain states, such as neuropathic pain and inflammation, nociceptors develop increased sensitivity to norepinephrine, and peripheral antinociception is likely mediated through these peripheral alpha2-adrenergic receptors.17,18
Clonidine has been used for intra-articular, epidural, intrathecal, intravenous regional, and peripheral nerve blocks in people.17,18 Medetomidine provided effective analgesia when administered epidurally in goats, cows, dogs, and cats and extended the duration of radial nerve blockade with mepivacaine in dogs.15,19-22 Dexmedetomidine (Dexdomitor—Pfizer Animal Health) has potentiated and prolonged the effects of intrathecal and epidural local anesthetics in rats, sheep, guinea pigs, and people.23 Spinal administration of dexmedetomidine provided a powerful antinociceptive effect in dogs,24 and epidural dexmedetomidine was found to decrease the minimum alveolar concentration (MAC) of isoflurane in dogs.25 The addition of dexmedetomidine to the local anesthetic solution in intravenous regional anesthesia in people improved the quality of anesthesia and decreased analgesic requirements but had no effect on the sensory and motor blockade onset or duration.26 Sedation, bradycardia, and decreased cardiac output can occur from systemic absorption, so alpha2 agonists should not be used in hypovolemic patients or patients with impaired cardiovascular function.15,17,22,25
LOCAL AND REGIONAL BLOCKS
Strict adherence to sterile technique will prevent complications from infection. Always surgically prepare the skin, wear sterile gloves, and use only sterile needles, syringes, and catheters. Sterile skin preparation is not required for digital nerve blocks, but sterile needles and syringes should be used. To avoid complications from intravenous or intra-arterial injection of local anesthetics, always aspirate before injection. In addition, always calculate the maximum total dose for each patient, reducing the dose for debilitated, elderly, or neonatal patients.
Table 4 summarizes the indications, potential complications, drugs, dosages, and equipment required for each regional block technique described below.
Infiltration anesthesia
Infiltration anesthesia can be used during small laceration repair and small mass excision, as a line block before surgical incision, or before or after incision closure (Figure 1).27-30 The total volume of local anesthetic is deposited in multiple subcutaneous injections around the area to be desensitized. Always aspirate before each injection to ensure intravenous injection does not occur. Lidocaine injections are painful, so make subsequent needle insertions through desensitized skin. Sodium bicarbonate can be added to lidocaine in a 1:9 ratio of bicarbonate to lidocaine to reduce pain on injection.31,32

Figure 1. An incisional infiltration block administered after the closure of an abdominal incision in a dog. Four or five subcutaneous injections were made on each side of the incision, from the caudal to the cranial ends.
Splash blocks
A splash block refers to direct application of a local anesthetic to the site of interest, most commonly the body wall upon closure of the abdomen, the peritoneum intraoperatively, or the ovarian ligaments during an ovariohysterectomy. For this technique, 4 mg/kg of lidocaine or 2 mg/kg of bupivacaine is dripped from a syringe onto the area to be blocked, after flushing and suctioning the abdomen. These methods have been shown to reduce anesthetic requirements in some veterinary studies.28,29
Digital nerve blocks
These blocks are especially beneficial for onychectomies and will block the superficial branches of the radial nerve, the median nerve, and dorsal and palmar branches of the ulnar nerve, providing effective analgesia of a distal extremity.3,30 Because of its long duration of action, 0.5% bupivacaine is the drug of choice for this block, and it is often combined with lidocaine for immediate onset of the block. Do not use epinephrine because of the potential for ischemia in extremities.
Inject 0.2 to 0.4 mg/kg of local anesthetic subcutaneously in three sites (Figure 2): lateral and proximal to the accessory carpal pad, medial to the accessory carpal pad, and at the dorsal-medial aspect of the proximal carpus. Alternatively, a simple ring block proximal to the carpus will block these nerves, and, although hindlimb onychectomy is discouraged, a ring block can be used for this procedure as well. In addition, individual digits can be blocked by injecting the local anesthetic subcutaneously in a ring proximal to the digit.

Figure 2. The digital nerve block to provide effective analgesia for an onychectomy. Inject 0.2 to 0.4 mg/kg of the local anesthetic subcutaneously in three sites-lateral and proximal to the accessory carpal pad to block the dorsal branch of the ulnar nerve (A), medial to the accessory carpal pad to block the median nerve and palmar branch of the ulnar nerve (B), and at the dorsal-medial aspect of the proximal carpus to block the superficial branches of the radial nerve (C).
Intravenous regional nerve blocks
Intravenous regional anesthesia, or a Bier block, is a rapid and reliable method for producing short-term (< 90 minutes) anesthesia and muscle relaxation of a distal extremity and can be performed in anesthetized or sedated animals.2,3,30 Because it requires restricted movement for a period of time, dogs often tolerate the procedure with moderate sedation, while cats often require heavy sedation. Sicker patients often tolerate this technique with minimal sedation, as they usually accept restraint for longer periods. This technique is indicated for mass removal, wound management, surgical biopsy, or fracture repair of a distal extremity.
For this technique, place an intravenous catheter into a distal vein of a limb, usually the cephalic vein or the saphenous vein. Place a rubber tourniquet, or a blood pressure cuff attached to a sphygmomanometer, around the limb proximal to the intravenous catheter, and tighten it to completely occlude arterial blood flow (pressure must be greater than systolic arterial pressure) (Figure 3). The advantage to using the sphygmomanometer and blood pressure cuff is that you can measure the pressure required to occlude arterial flow, avoiding excessive pressure that may cause direct tissue trauma and ischemic damage. Limb exsanguination with an Esmarch bandage is often described in reference texts for this technique1,2 but, in our experience, is not required in dogs or cats to produce an effective block. Inject lidocaine or mepivacaine into the catheter (Table 4). Never use bupivacaine, as intravenous administration of bupivacaine is always contraindicated.

Figure 3. A Bier block provides excellent anesthesia to the extremity distal to the tourniquet as long as the tourniquet remains tightened. Lidocaine is being injected slowly into an intravenous catheter.
Five to 10 minutes are required to achieve surgical anesthesia distal to the tourniquet, which will last up to 90 minutes. To avoid ischemic tissue damage, do not leave the tourniquet in place for more than 90 minutes.1,2 Sensation will return within five to 10 minutes of removing the tourniquet, and residual analgesia is minimal (20 to 30 minutes), so provide other analgesics postoperatively.2 This technique provides a blood-free surgical site and is also used with injectable antibiotics to obtain high tissue concentrations in a distal extremity.33,34 This technique is associated with few side effects as there is minimal systemic absorption of local anesthetic as long as the tourniquet remains in place and prevents blood flow to and venous return from the extremity.1,2 It is important to ensure that the tourniquet is not dislodged too early, as this will result in rapid plasma uptake of the anesthetic. Using lidocaine or mepivacaine doses below the toxic doses (Tables 2 & 4) will minimize the possibility of toxicosis should the tourniquet become dislodged.
The mechanism by which local anesthetics produce intravenous regional anesthesia is unknown but probably results from local diffusion of the anesthetic and the blockade of nerve endings and nerve trunks and from leakage under the cuff, resulting in systemic absorption.1 Some systemic absorption is also thought to occur from interosseous vessels.35
Soaker-type catheter placement
A soaker-type catheter, also referred to as a diffusion or wound catheter, is simply fenestrated tubing that is sterilely placed at a painful site for the continuous or intermittent administration of local anesthetics. Soaker-type catheters are easily placed during a surgical procedure, such as a limb amputation or large tumor resection, just before closure. In addition, they can be positioned nonsurgically at the site of a lesion that is painful but cannot be resected or when a course of palliative care has been chosen.
Efficacy and adverse effects. The veterinary literature regarding the use of soaker-type catheters is limited, but human medical experience is extensive and, for the most part, positive. A 2007 study demonstrated the viability of soaker-type catheters in postoperative pain management in dogs, cats, and goats.36 In another veterinary study, continuous infusion of bupivacaine into normal dogs' stifles for eight hours demonstrated plasma concentrations well below the toxic dose.37 Unfortunately, no studies have evaluated the efficacy of continuous infusion of local anesthetics in veterinary patients with surgical or traumatic wounds. Results from human trials are largely encouraging, with most showing an improvement in patient pain scores or a decrease in opioid requirements,38-46 whereas others have not found a benefit.47-50 Of great interest is the reduction in chronic pain in people a minimum of four years after bone graft harvesting with the use of continuous bupivacaine infusion at the graft site for 48 hours.51
Divergent conclusions about the utility of soaker-type catheters may be due to different catheter placement depths (fascial layers vs. subcutaneous tissues), study end points (opioid consumption vs. length of hospital stay or patient satisfaction), innervation at various surgical sites (inguinal region vs. sternum), and other study design disparities. Few serious adverse effects attributable to local anesthetic infiltration are reported in veterinary patients. One case of lidocaine toxicosis with continuous infusion of 3 mg/kg/hr for three days has been described in a dog36 ; additional complications could include infection, hematoma formation, intravascular injection and subsequent cardiovascular collapse, or intraneural administration of local anesthetics and resulting nerve damage.

Figure 4. A commercially available soaker-type catheter and drug reservoir; the catheter has been inserted into the soft tissue over the humerus of a dog with osteosarcoma to provide palliative analgesia.
Obtaining a catheter. Soaker-type catheters can be purchased commercially (Diffusion/Wound Catheter—MILA International; On-Q PainBuster Post-Op Relief System—I-Flow Corp) (Figure 4) or can be fashioned in a sterile manner from materials commonly found in the veterinary clinic. Commercial catheters are made of plastic tubing, often polyurethane, and typically range in length from 2.5 to 10 in. The fenestrated areas vary in length and are designed to spread local anesthetic over a predetermined area (5 to 22 cm).
Homemade catheters are readily constructed intraoperatively.52,53 For instructions on how to make a soaker-type catheter, see the boxed text "How to make a soaker-type catheter." The catheter can be made ahead of time and gas-sterilized with either hydrogen peroxide or ethylene oxide if facilities are available.
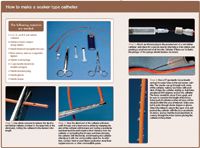
How to make a soaker-type catheter
Placing the catheter. Intraoperative placement of either a commercially manufactured or homemade soaker-type catheter is quick and easy, being similar in nature to placing a drain during closure. Place the catheter in the deepest layer of the wound, and make sure all fenestrations are within the muscle layers or subcutaneous tissues. Loose tacking absorbable sutures can be used in the deep layer, but the catheter should slide out easily for removal. If a drain is also to be placed, position the soaker-type catheter dorsally and the drain ventrally. The catheter can be tacked to the skin with suture to keep it in place and then bandaged as necessary (Figure 5).

Figure 5. A red rubber soaker-type catheter in place, along with a wound drain, in a dog that underwent radical excision of a soft tissue sarcoma. Note that the catheter is placed dorsally in the wound. A tacking suture holds the catheter to the skin, and the catheter will be wrapped to further secure it to the dog. Bupivacaine (1 mg/kg) will be administered through the catheter every six hours.
Soaker-type catheter placement can be accomplished outside the operating room as well when a painful lesion is not to be surgically addressed. Commercially available catheters are advantageous in such situations because they have tear-away applicators that allow for minimal tissue trauma during placement. Homemade versions could also be placed in such a situation but would require some tissue dissection to appropriately localize the catheter. Tunneling the catheter some distance in the subcutaneous tissues before exiting the skin will help provide stability to the placement.
Elastomeric and electronic reservoirs that allow for continuous infusion of local anesthetic can be purchased from the same companies that supply commercial soaker-type catheters. Syringe pumps can also be used to provide continuous infusion. Lidocaine or mepivacaine are likely the safest choices for continuous infusion, and care should be taken to avoid toxic doses, especially in cats. Infusions of lidocaine or mepivacaine of 1 to 2 mg/kg/hr should be safe and effective in most cases. For intermittent administration, bupivacaine at 1 to 2 mg/kg is the best option because of its long duration of action (four to six hours). Catheters are typically left in place for one to three days, but can be left in longer if strict aseptic technique is followed.
SUMMARY
The techniques described above are easy to perform and require simple materials and drugs available in most small-animal veterinary practices. By providing preemptive and multimodal analgesia, reducing the need for systemic analgesics and anesthetics and the attendant side effects, and decreasing the perioperative stress response through the use of local anesthetic techniques, you can improve the overall quality of the analgesic care in your patients. Look for subsequent articles in this series throughout the year covering additional helpful and easy-to-perform anesthetic techniques.
ACKNOWLEDGMENT
The authors wish to thank Gregory Hirshoren, Instructional Resources, College of Veterinary Medicine, The University of Tennessee, for the photos that accompany this article.
Christine Egger, DVM, MVSc, DACVA
Lydia Love, DVM
Department of Small Animal Clinical Sciences
College of Veterinary Medicine
The University of Tennessee
Knoxville, TN 37996
REFERENCES
1. Stoelting RK, Hillier SC. Local anesthetics. In: Pharmacology and physiology in anesthetic practice. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 2006;179-207.
2. Scarda RT, Tranquilli WJ. Local anesthetics; Local and regional anesthesia and analgesia: dogs; Local and regional anesthesia and analgesia: cats. In: Lumb and Jones' veterinary anesthesia and analgesia. 4th ed. Tranquilli WJ, Thurmon JC, Grimm KA, eds. Iowa, Ames: Wiley-Blackwell, 2007.
3. Lemke KA. Pain management II: local and regional anaesthetic techniques. In: Seymour C, Duke-Novakovski T, eds. BSAVA manual of canine and feline anaesthesia and analgesia. 2nd ed. Gloucester, UK: British Small Animal Veterinary Association, 2007;104-114.
4. Yaksh TL. Pharmacology and mechanisms of opioid analgesic activity. Acta Anaesthesiol Scand 1997;41(1 Pt 2):94-111.
5. Stein C, Machelska H, Schafer M. Peripheral analgesic and anti-inflammatory effects of opioids. Z Rheumatol 2001;60:416-424.
6. Kapitzke D, Vetter I, Cabot PJ. Endogenous opioid analgesia in peripheral tissues and the clinical implications for pain control. Ther Clin Risk Manag 2005;1(4):279-297.
7. Axelsson K, Gupta A, Johanzon E, et al. Intraarticluar administration of ketorolac, morphine, and ropivacaine combined with intraarticular patient-controlled regional analgesia for pain relief after shoulder surgery: a randomized, double-blind study. Anesth Analg 2008;106(1):328-333.
8. Kona-Boun JJ, Cuvelliez S, Troncy E. Evaluation of epidural administration of morphine or morphine and bupivacaine for postoperative analgesia after premedication with an opioid analgesic and orthopedic surgery in dogs. J Am Vet Med Assoc 2006;229(7):1103-1112.
9. Day TK, Pepper WT, Tobias TA, et al. Comparison of intra-articular and epidural morphine for analgesia following stifle arthrotomy in dogs. Vet Surg 1995;24(6):522-530.
10. Jadon A, Panigrahi MR, Parida SS, et al. Buprenorphine improves the efficacy of bupivacaine in nerve plexus block: a double blind randomized evaluation in subclavian perivascular brachial block. Internet J Anesth 2008;16(2).
11. Candido KD, Winnie AP, Ghaleb AH, et al. Buprenorphine added to the local anesthetic for axillary brachial plexus block prolongs postoperative analgesia. Reg Anesth Pain Med 2002;27(2):162-167.
12. Lanz E, Simko G, Theiss D, et al. Epidural buprenorphine—a double-blind study of postoperative analgesia and side effects. Anesth Analg 1984;63(6):593-598.
13. Bazin JE, Massoni C, Bruelle P, et al. The addition of opioids to local anaesthetics in brachial plexus block: the comparative effects of morphine, buprenorphine and sufentanil. Anaesthesia 1997;52(9):858-862.
14. Pypendop BH, Siao KT, Pascoe PJ, et al. Effects of epidurally administered morphine or buprenorphine on the thermal threshold in cats. Am J Vet Res 2008;69(8):983-987.
15. Lamont LA, Lemke KA. The effects of medetomidine on radial nerve blockade with mepivacaine in dogs. Vet Anaesth Analg 2008;35(1):62-68.
16. McCartney CJ, Duggan E, Apatu E. Should we add clonidine to local anesthetic for peripheral nerve blockade? A qualitative systemic review of the literature. Reg Anesth Pain Med 2007;32(4):330-338.
17. Gabriel JS, Gordin V. Alpha 2 agonists in regional anesthesia and analgesia. Curr Opin Anaesthesiol 2001;14(6):751-753.
18. Forster JG, Rosenberg PH. Clinically useful adjuvants in regional anaesthesia. Curr Opin Anaesthesiol 2003;16(5):477-486.
19. Mpanduji DG, Bittegeko SB, Mgasa MN, et al. Analgesic, behavioural and cardiopulmonary effects of epidurally injected medetomidine (Domitor) in goats. J Vet Med A Physiol Pathol Clin Med 2000;47(2):65-72.
20. Lin HC, Trachte EA, DeGraves FJ, et al. Evaluation of analgesia induced by epidural administration of medetomidine to cows. Am J Vet Res 1998;59(2):162-167.
21. Vesal N, Cribb PH, Frketic M. Postoperative analgesic and cardiopulmonary effects in dogs of oxymorphone administered epidurally and intramuscularly, and medetomidine administered epidurally: a comparative clinical study. Vet Surg 1996;25(4):361-369.
22. Duke T, Cox AM, Remedios AM, et al. The analgesic effects or administering fentanyl or medetomidine in the lumbosacral epidural space of cats. Vet Surg 1994;23(2):143-148.
23. Schug SA, Saunders D, Kurowski I, et al. Neuraxial drug administration: a review of treatment options for anaesthesia and analgesia. CNS Drugs 2006;20(11);917-933.
24. Sabbe MB, Penning JP, Ozaki GT, et al. Spinal and systemic action of the alpha 2 receptor agonist dexmedetomidine in dogs. Antinociception and carbon dioxide response. Anesthesiology 1994;80(5):1057-1072.
25. Campagnol D, Teixeira Neto FJ, Giordano T, et al. Effects of epidural administration of dexmedetomidine on the minimum alveolar concentration of isoflurane in dogs. Am J Vet Res 2007;68(12):1308-1318.
26. Esmaoglu A, Mizrak A, Akin A, et al. Addition of dexmedetomidine to lidocaine for intravenous regional anaesthesia. Eur J Anaesthesiol 2005;22(6):447-451.
27. Savvas I, Papazoglou LG, Kazakos G, et al. Incisional block with bupivacaine for analgesia after celiotomy in dogs. J Am Anim Hosp Assoc 2008;44(2):60-66.
28. Carpenter RE, Wilson DV, Evans AT. Evaluation of intraperitoneal and incisional lidocaine or bupivacaine for analgesia following ovariohysterectomy in the dog. Vet Anaesth Analg 2004;31(1):46-52.
29. Zilberstein LF, Moens YP, Leterrier E. The effect of local anaesthesia on anaesthetic requirements for feline ovariectomy. Vet J 2008;178(2):214-218.
30. Gaynor JS, Mama KR. Local and regional anesthetic techniques for alleviation of perioperative pain. In: Gaynor J, Muir W, eds. Handbook of veterinary pain management. St Louis, Mo: Mosby, 2002;261-280.
31. Matsumoto AH, Reifsnyder AC, Hartwell GD, et al. Reducing the discomfort of lidocaine administration through pH buffering. J Vasc Interv Radiol 1994;5(1):171-175.
32. Vossinakis IC, Stavroulaki P, Paleochorlidis I, et al. Reducing the pain associated with local anaesthetic infiltration for open carpal tunnel decompression. J Hand Surg [Br] 2004;29(4):399-401.
33. Gilliam JN, Streeter RN, Papich MG, et al. Pharmacokinetics of florfenicol in serum and synovial fluid after regional intravenous perfusion in the distal portion of the hind limb of adult cows. Am J Vet Res 2008;69(8):997-1004.
34. Fiorello CV, Beagley J, Citino SB. Antibiotic intravenous regional perfusion for successful resolution of distal limb infections: two cases. J Zoo Wildl Med 2008;39(3):438-444.
35. Coleman MM, Peng PW, Regan JM, et al. Quantitative comparison of leakage under the tourniquet in forearm versus conventional intravenous regional anesthesia. Anesth Analg 1999;89(6):1482-1486.
36. Abelson AL, Blaze, CA, McCobb EC, et al. Use of a wound soaker catheter for the administration of local anesthetic for post-operative analgesia: 56 cases (abst), in Proceedings. Int Vet Emerg Crit Care Symp 2007.
37. Bubenik L, Hosgood G, Barker S, et al. Estimated plasma bupivacaine concentration after single dose and eight-hour continuous intra-articular infusion of bupivacaine in normal dogs. Vet Surg 2007;36(8):783-791.
38. Beaussier M, El'Ayoubi H, Schiffer E, et al. Continuous preperitoneal infusion of ropivacaine provides effective analgesia and accelerates recovery after colorectal surgery: a randomized, double-blind, placebo-controlled study. Anesthesiology 2007;107(3):461-468.
39. Cheong WK, Seow-Choen F, Eu KW, et al. Randomized clinical trial of local bupivacaine perfusion versus parenteral morphine infusion for pain relief after laparotomy. Br J Surg 2001;88(3):357-359.
40. Chiu KM, Wu CC, Wang MJ, et al. Local infusion of bupivacaine combined with intravenous patient-controlled analgesia provides better pain relief than intravenous patient-controlled analgesia alone in patients undergoing minimally invasive cardiac surgery. J Thorac Cardiovasc Surg 2008;135(6):1348-1352.
41. Dowling R, Thielmeier K, Ghaly A, et al. Improved pain control after cardiac surgery: results of a randomized, double-blind, clinical trial. J Thorac Cardiovasc Surg 2003;126(5):1271-1278.
42. Fredman B, Shapiro A, Zohar E, et al. The analgesic efficacy of patient-controlled ropivacaine instillation after Cesarean delivery. Anesth Analg 2000;91(6):1436-1440.
43. White PF, Rawal S, Latham P, et al. Use of a continuous local anesthetic infusion for pain management after median sternotomy. Anesthesiology 2003;99(4):918-923.
44. Gottschalk A, Burmeister MA, Radtke P, et al. Continuous wound infiltration with ropivacaine reduces pain and analgesic requirement after shoulder surgery. Anesth Analg 2003;97(4):1086-1091.
45. Mecklem DW, Humphrey MD, Hicks RW. Efficacy of bupivacaine delivered by wound catheter for post-Caesarean section analgesia. Aust N Z J Obstet Gynaecol 1995;35(4):416–421.
46. Baig MK, Zmora O, Derdemezi J, et al. Use of the ON-Q pain management system is associated with decreased postoperative analgesic requirement: double blind randomized placebo pilot study. J Am Coll Surg 2006;202(2):297-305.
47. Boss AP, Maurer T, Seiler S, et al. Continuous subacromial bupivacaine infusion for postoperative analgesia after open acromioplasty and rotator cuff repair: preliminary results. J Shoulder Elbow Surg 2004;13(6):630-634.
48. Fredman B, Zohar E, Tarabykin A, et al. Bupivacaine wound instillation via an electronic patient-controlled analgesia device and a double-catheter system does not decrease postoperative pain or opioid requirements after major abdominal surgery. Anesth Analg 2001;92(1):189-193.
49. Magnano D, Montalbano R, Lamarra M, et al. Ineffectiveness of local wound anesthesia to reduce postoperative pain after median sternotomy. J Card Surg 2005;20(4):314-318.
50. Polglase AL, McMurrick PJ, Simpson PJ, et al. Continuous wound infusion of local anesthetic for the control of pain after elective abdominal colorectal surgery. Dis Colon Rectum 2007;50(12):2158-2167.
51. Singh K, Phillips FM, Kuo E, et al. A prospective, randomized, double-blind study of the efficacy of postoperative continuous local anesthetic infusion at the iliac crest bone graft site after posterior spinal arthrodesis: a minimum of 4-year follow-up. Spine 2007;32(25):2790-2796.
52. Hansen B. Management of pain in the critically ill, in Proceedings. Int Vet Emerg Crit Care Symposium 2003.
53. Lascelles BDX. Pain management in acute cancer care: use of wound analgesic catheters, in Proceedings. Br Small Anim Vet Congress 2007.