Managing the common comorbidities of feline urethral obstruction
Anticipate and treat these seven conditions that can result from urethral obstruction.
The blocked male cat is a common case in both general and emergency veterinary practice. At one university teaching hospital, 9% of the annual feline emergency caseload was made up of male cats with urethral obstructions.1 Basic treatment of this condition typically involves passing a urethral catheter and relieving the obstruction, a skill that is readily learned when such cases present. However, true excellence comes when a practitioner can anticipate and treat the comorbidities most commonly associated with this disease.

(Tetra Images/Getty Images)
Comorbidities of urethral obstruction in male cats can be divided into two categories: those that exist at the time of presentation and those that develop during the course of treatment. In this article, I will review the causes of and treatment approach for seven of the most common concurrent morbidities in blocked male cats.
PROBLEMS THAT EXIST AT PRESENTATION
Azotemia
Azotemia in blocked cats is classically attributed to prerenal and postrenal causes. Because the cat is unable to urinate (postrenal component), the pressure in the bladder, ureters, and kidneys increases.2 When the intratubular pressure in the kidney increases, the kidney's glomerular filtration rate (GFR) and therefore its ability to filter toxins (including blood urea nitrogen [BUN] and creatinine) decreases.2 This leads to an increase in blood concentrations of these toxins. Additionally, cats that are azotemic may feel nauseated and inappetent, leading to fluid loss from vomiting and decreased intake of water and food. The resulting dehydration causes prerenal azotemia.
Treating azotemia. Treatment for azotemia involves relieving the obstruction to allow urine flow out of the bladder and administering crystalloid fluids. When a urinary catheter is placed, urine can flow and reestablish GFR. This leads to filtration and elimination of the BUN, creatinine, and other waste products from the bloodstream. Additionally, fluid administration dilutes the BUN and creatinine concentrations, as well as improves GFR to increase the filtration rate of toxins. The most efficient route of fluid administration is intravenous. Subcutaneous fluids are less effective than intravenous fluids because they are usually given in smaller quantities and at a slower rate.
Hyperkalemia
An estimated 12% of blocked cats present with hyperkalemia, which can range from clinically insignificant ([K+] 5 to 6 mEq/L) to fatal ([K+] ≥ 9 mEq/L).1 Potassium increases secondary to decreased GFR, which causes ineffective excretion of potassium from the kidneys in the distal tubules as well as an inability of the kidneys to excrete the potassium in the urine.3 Because this is a potentially deadly problem, measure serum potassium concentrations in every patient with urethral obstruction.
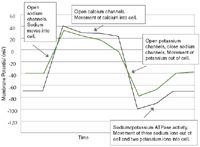
Figure 1. The normal cardiac cell action potential (black line). The normal resting cell membrane potential is approximately -70 mV. The normal threshold cell membrane potential is approximately -50 mV. All cells at rest have high intracellular potassium concentrations and high extracellular sodium concentrations. All channels allow for movement of ions from an area of high concentration to an area of low concentration. The green line indicates alterations that occur when the body is hyperkalemic.
As potassium concentration rises, the body reacts by moving potassium intracellularly through the effects of insulin, epinephrine, and the increased potassium concentration in the extracellular fluid.3 Additionally, the body increases renal excretion of potassium through the effects of aldosterone.3-5 Increases in the intracellular concentration of potassium cause the resting membrane potential to become less negative (i.e. greater than the standard resting membrane potential of -70 mV) (Figure 1). The increased resting membrane potential inactivates both fast sodium channels (making it more difficult for the cell to depolarize) and sodium/potassium ATPase pumps, which typically work to maintain the normal gradient of sodium and potassium on either side of the cell membrane.5 When the cells of the atria are affected, they become unable to control automaticity of the heart and arrhythmias can result (Table 1), culminating in sinus arrest, a ventricular escape rhythm, and death.
In clinical cases, the classic arrhythmias are often not seen at all or are seen at unexpected potassium concentrations. This is because other metabolic abnormalities—such as hypocalcemia, acidosis, and hypermagnesemia—can interact with potassium or can directly affect ECG results. Hypocalcemia prolongs the plateau phase of the action potential, resulting in prolongation of the S-T and Q-T intervals.3,5 In one study, 34% of obstructed cats were hypocalcemic.2 Acidosis, which occurs in about 40% of obstructed cats, occurs because of the acidifying effects of the uremic acids coupled with an inability to excrete hydrogen ions.2 The body reacts to acidosis by moving hydrogen ions into cells in exchange for moving potassium ions out of cells, thus increasing serum potassium concentrations and potentially altering the ECG. Acidosis also causes release of calcium into the bloodstream, which alters ECG findings.5 Finally, some obstructed animals have increased serum magnesium concentrations, which also can alter the ECG results.5
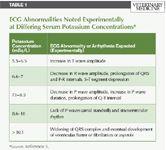
Table 1 ECG Abnormalities Noted Experimentally at Differing Serum Potassium Concentrations*
Treating hyperkalemia. The definitive treatment for hyperkalemia is to reestablish urine flow and GFR either by passing a urinary catheter or otherwise diverting or removing the urine. Other treatments for hyperkalemia involve intravenous fluid therapy alone or in addition to drugs. Drug options for hyperkalemia include dextrose or insulin and dextrose (to reduce the serum potassium concentrations), sodium bicarbonate (to reduce the serum potassium concentrations), or calcium gluconate (to reduce the effects of hyperkalemia on the heart). See Table 2 for dosing recommendations.

Table 2 Drug Dosages for Treating Hyperkalemia
Intravenous fluids dilute the potassium and lower its serum concentration. In addition, fluids increase excretion through the kidneys by increasing GFR. In cases in which the obstruction was easily removed and the cat seems metabolically stable (no cardiac effects; cat is not obtunded), fluids may be the only treatment required to reduce the potassium.
Administration of dextrose (which stimulates endogenous insulin production by pancreatic beta cells) or insulin with dextrose leads to insulin binding to its receptor. This in turn activates the sodium/potassium ATPase pump, which moves potassium into the cell, transiently reducing hyperkalemia and reestablishing the extracellular to intracellular potassium gradient so that cells can repolarize and therefore depolarize again.4
Sodium bicarbonate is given to reduce the pH in the extracellular space. This stimulates the exchange of intracellular hydrogen ions for extracellular potassium ions to reduce the pH in the extracellular space.4 The exact mechanism for this exchange is unknown, but the net effect is to move potassium into the cell, again reestablishing the extracellular to intracellular potassium gradient.4 Calcium gluconate works differently—it increases the cell's threshold membrane potential and, thus, reestablishes the cell's ability to normally depolarize despite its increased resting membrane potential.3 Calcium gluconate does not directly alter the serum potassium concentrations.
While all these treatments will work to protect against the ill effects of excessive potassium, sodium bicarbonate has the highest risk of creating iatrogenic complications and should be avoided in all but severely acidotic patients (i.e. pH < 7.1).
COMPLICATIONS THAT OCCUR DURING TREATMENT
Postobstructive diuresis
Postobstructive diuresis (POD) is a long-recognized complication that is most common in animals that have had a urethral obstruction for a long period.6 When it occurs, the patient produces a large amount of urine that greatly exceeds the volume of fluids being administered. In some cases, POD can lead to severe dehydration, hypovolemia, and shock.6 In a recent study, 46% of obstructed cats had POD during the first six hours after the obstruction was removed.7 Although which cats will develop POD cannot be predicted, a pH below 7.35 (i.e. acidosis) correlates with the presence of POD.7 POD also occurs in animals that have been obstructed longer and are more clinically affected.7
Three reasons for POD have been reported: urea diuresis, salt diuresis, and water diuresis. Urea diuresis occurs when BUN concentrations increase secondary to decreased GFR. When the patient has been catheterized and urine flow has been reestablished, the kidneys filter and excrete the urea load, leading to massive losses of water along with the urea.6,8,9 Salt diuresis is similar except that excess sodium rather than urea is excreted along with massive amounts of water when the obstruction is relieved.6,9,10 Water diuresis is a short-term and transient nephrogenic diabetes insipidus that occurs when the collecting tubule in the kidney becomes temporarily unresponsive to antidiuretic hormone and cannot reabsorb water.6
In all cases of POD, the kidneys lose their ability to reabsorb sodium and water secondary to the obstruction and loss of the medullary gradient occurs, which promotes water loss from the kidneys.8 Other factors contributing to POD include increases in total body water due to the inability to urinate8,9 and a buildup of urea and other solutes within the renal tubules, which induces an osmotic diuresis.9,10
Managing POD. Management of POD requires monitoring urine production and matching it to the rate of intravenous fluid administration. This is accomplished by using a closed urinary collection system and measuring the volume of urine produced. Urine is typically measured every four to six hours and the total volume of urine is divided by the time over which it was produced to determine the total milliliters of urine per hour (ml/hr). The fluid pump should then be set to that same ml/hr until the next urine measurement time point. Thus, the fluid rate is always changed in reaction to the previous amount of urine production. It is important not to be afraid of extremely high fluid rates in these patients (in some cases upwards of 100 ml/hr for a standard sized cat). Not matching the urine output is more detrimental to these patients than unwarranted concerns about fluid-overloading because insufficient fluid replacement can lead to dehydration and worsening prerenal azotemia.
The duration of POD varies, but anecdotally seems to last 24 to 48 hours in most cases. Evaluate several factors to determine whether the POD has resolved. First, the measured urine production will match the administered intravenous fluids for several consecutive measurement periods. Second, the urine will appear grossly normal and dilute without blood contamination. Third, when the intravenous fluid rate is reduced, the next urine measurement will also be reduced to match the amount of fluid administered. If the measured urine amount is higher than the administered fluids, the POD is still ongoing and the fluid rate should be increased again to match the urine production. In a recent study, some cats still displayed POD 84 hours after the obstruction was removed.7
Urethral tear
Urethral tears are rare in cats, estimated to occur in 0.6% of the total number of cats with lower urinary tract disease (including both obstructed and nonobstructed cats).11 Tearing is most often iatrogenic, caused by manipulating a urethral catheter.11 Once the urethra is torn, urine leaks into the subcutaneous tissues causing severe inflammation.
Clinical signs can include pain in the perineal and preputial regions, swelling in the preputial and surrounding areas, or severely inflamed and even necrotic skin at the site of the subcutaneous urine leakage (typically the perineal or scrotal and preputial region).12 Other signs reported include hematuria, anorexia, and depression.12 A urethral tear can be difficult to diagnose when it occurs because cats may display only vague clinical signs. It is important to recognize that cats may not show any changes in urination and may be able to urinate normally.12
Managing tears. A torn urethra can be managed in several ways, all centered on the basic concept of preventing contact of urine with the urethra while it heals. This eliminates the complications of skin necrosis and inflammation secondary to the caustic effects of the urine and reduces periurethral inflammation secondary to urine leakage.13 One method of urine diversion is to simply keep a urinary catheter in place until the urethra heals.11,13 This catheter can be carefully placed through the urethra in the normal retrograde fashion or can be placed using a guidewire that is introduced (via cystotomy) from the bladder, directed normograde out the urethra, and used to guide a catheter from the urethra into the bladder ('inside to outside technique").12
Other methods of urinary diversion involve placing a cystostomy tube through the skin into the bladder. The traditional method of tube cystostomy placement involves a caudal ventral midline approach where the entire bladder is visualized and a tube is placed through a purse-string suture on the ventral bladder surface and exited through a paramedian incision on the cat's ventral abdomen.14 The tube used for this technique is usually a mushroom-tipped urinary catheter that is emptied at least four times a day to keep the bladder small so that urine does not travel down the urethra.
Newer published techniques for cystostomy tube placement involve a minimally invasive approach in which the bladder is entered through the lateral aspect of the flank.15 The entire bladder is not visualized with this technique; only a portion of the bladder wall is seen through the incision. A mushroom-tipped catheter is placed through a purse-string suture into the portion of the bladder wall seen through the incision, and the tube exits dorsal to the incision site on the lateral abdomen.
Laparoscopy has also been used to place a percutaneous Foley catheter in dogs16 and a transcutaneous pigtail catheter (silicone balloon catheter with a pigtail tip) in sheep17 to allow for urine diversion. In people, similar pigtail catheters have been placed percutaneously into the bladder with ultrasound guidance.18
Healing time of the urethra can range from several days to a week or more (reported as five to 14 days in a recent study).12 The patency of the urethra can be periodically evaluated by a contrast urethrogram (i.e. injecting contrast medium from a catheter that is pulled out to the most distal portion of the urethra and looking for leakage into the tissues surrounding the urethra).11 Typical contrast agents used are noniodinated agents such as iohexol or diatrizoate meglumine and diatrizoate sodium solution (MD-76R—Mallinckrodt) administered at a maximal dosage of 5 ml/cat. Once a contrast agent can be successfully injected from the tip of the penis into the bladder without any leakage, the urethra is healed and the catheter or cystotomy tube can be removed.
Detrusor atony
Detrusor atony is a condition that occurs in previously obstructed cats after excessive expansion of the urinary bladder.19 In this condition, the tight junctions of the smooth muscle in the bladder become stretched or torn apart, resulting in weak, uncoordinated, or completely absent contractions of the bladder muscle.2,19 Cats with this complication usually have a persistently large bladder that may or may not be easily expressed.
Treating atony. Once recognized, treatment for this condition is straightforward and involves keeping the bladder small to allow the tight junctions to heal. This can be accomplished by regular manual expression of the bladder or placement of a urinary catheter. Pharmacologic intervention with bethanechol (1.25 to 7.5 mg/cat orally, every eight hours) or cisapride (0.5 mg/kg orally, b.i.d. or t.i.d.) until normal bladder function has returned (anywhere from a few days to a few weeks) can also be considered. Bethanechol activates the muscarinic receptors in the detrusor muscle (parasympathetic stimulation) causing contraction. Cisapride increases the release of acetylcholine to facilitate binding to muscarinic receptors and induce parasympathetic-induced contraction of the bladder. In the normal micturition reflex, sympathetic innervation from the spinal cord simultaneously causes relaxation of the internal urethral sphincter.19,20 Therefore, if bethanechol or cisapride is administered, it is imperative that the patient also be given a separate drug to relax the urethral sphincter to facilitate bladder emptying. (See urethral hyperactivity below.)
Urethral hyperactivity
In some cases, urethral spasms in cats may be a cause of functional obstruction.2 Clinically, these cats appear to be straining to urinate and pass only small amounts of urine. However, urine can be expressed from these cats relatively easily because there is no physical obstruction.
Urethral edema and inflammation commonly develop in obstructed cats due to catheterization and the presence of the catheter, and they are likely the cause of smooth and skeletal muscle spasms along the urethra's length.2,21 The concern in patients displaying urethral hyperactivity is that they are unable to completely express their bladders and will require recatheterization.
Though it might seem that an obvious treatment for edema and inflammation would be an anti-inflammatory drug (a glucocorticoid or NSAID), there is no published evidence that these medications reduce urethral inflammation. Also, with the well-documented fact that both corticosteroids and NSAIDS can be detrimental in patients that are dehydrated or that have any sort of renal dysfunction, there is no good support for the use of these drugs in cases of urethral obstruction.
Treating urethral hyperactivity. Therefore, treatments for urethral hyperactivity center on the use of the smooth muscle relaxants prazosin and phenoxybenzamine. The preprostatic urethra in male cats is primarily smooth muscle, whereas the postprostatic region is primarily skeletal muscle.21 Prazosin (0.25 to 0.5 mg/cat orally, every 12 to 24 hours) is a selective alpha-1 antagonist, and phenoxybenzamine (2.5 to 10 mg/cat orally, divided one to two times daily) is a nonspecific alpha antagonist. Alpha receptors control the contraction of smooth muscle, and therefore these medications are aimed at relaxing smooth muscle in the bladder neck and preprostatic urethra to enhance urine flow.22 Both medications can be given orally to cats but can cause hypotension in sensitive cats or when given at higher dosages. Clinical studies do not strongly support the efficacy of these medications in cats, but both are used commonly in clinical cases.21,22 Some experimental evidence indicates that dantrolene, a skeletal muscle relaxant, in combination with prazosin, may reduce urethral muscle tone in cats.21
Reobstruction
Some cats experience reobstruction in short order after the urinary catheter is removed. Anecdotally, reobstruction occurs in a large percentage of cats, most commonly in the first 24 hours after urinary catheter removal. One study describing 41 cats with urethral obstruction indicated that 14 cats (36%) had reobstruction within about two years' time (with the majority experiencing reobstruction within six months).23
Handling reobstruction. No data directly support the best plan of action for cats that have recurrent obstruction. However, clinicians generally recommend additional procedures to owners after a cat has become obstructed twice, especially in short order (i.e. within days to weeks). The most commonly recommended procedure for these cats is a perineal urethrostomy. This surgery is aimed at permanently widening and shortening the urethra to prevent reobstruction. Anecdotally, patients undergoing this surgery are at a very low risk of reobstruction. No reobstruction was reported within four years in a recent study of 59 cats that had perineal urethrostomy.24
CONCLUSION
Urethral obstruction in male cats has a high morbidity rate. However, this condition should not have a high mortality rate. While relieving the obstruction with catheterization is the definitive treatment, practitioners need to be prepared to identify and treat the conditions that coexist with urethral obstruction. Anticipation of these complications, coupled with competent treatment, results in a very low mortality rate in afflicted male cats.
Elizabeth J. Thomovsky, DVM, MS, DACVECC
Department of Medical Sciences
School of Veterinary Medicine
University of Wisconsin-Madison
Madison, WI 53706
REFERENCES
1. Lee JA, Drobatz KJ. Characterization of the clinical characteristics, electrolytes, acid-base, and renal parameters in male cats with urethral obstruction. J Vet Emerg Crit Care 2003;13(4):227-233.
2. Bartges JW, Delmar RF, Polzin DJ, et al. Pathophysiology of urethral obstruction. Vet Clin North Am Small Anim Pract 1996;26(2):255-264.
3. DiBartola SP, de Morais HA. Disorders of potassium: hypokalemia and hyperkalemia. In: DiBartola SP, ed. Fluid, electrolyte, and acid base disorders in small animal medicine. 3rd ed. St. Louis, Mo: Elsevier, 2006;91-121.
4. Giebisch G, Windhager E. Transport of potassium. In: Boron WF, Boulpaep EL, eds. Medical physiology: a cellular and molecular approach. Philadelphia, Pa: Elsevier, 2005;814-827.
5. Tag TL, Day TK. Electrocardiographic assessment of hyperkalemia in dogs and cats. J Vet Emerg Crit Care 2008;18(1):61-67.
6. Baum N, Anhalt M, Carlton Jr CE, et al. Post obstructive diuresis. J Urol 1974;114:53-56.
7. Francis BJ, Wells RJ, Rao S, et al. Retrospective study to characterize post-obstructive diuresis in cats with urethral obstruction. J Fel Med Surg 2010;12:606-608.
8. Sophasan S, Sorrasuchart S. Factors inducing post-obstructive diuresis in rats. Nephron 1984;38:125-133.
9. Gross JB, Kokko JP. The influence of increased tubular hydrostatic pressure on renal function. J Urol 1976;115:427-432.
10. Harris RH, Yarger WE. Pathogenesis of post-obstructive diuresis: the role of circulating natriuretic and diuretic factors, including urea. J Clin Invest 1975;56:880-887.
11. Osborne CA, Sanderson SL, Lulich JP, et al. Medical management of iatrogenic rents in the wall of the feline urinary bladder. Vet Clin North Am Small Anim Pract 1996; 26(3):551-562.
12. Meige F, Sarrau S, Autefage A. Management of traumatic urethral rupture in 11 cats using primary alignment with a urethral catheter. Vet Comp Orthop Traumatol 2008;21:76-84.
13. Anderson RB, Aronson LR, Drobatz KJ, et al. Prognostic factors for successful outcome following urethral rupture in dogs and cats. J Am Anim Hosp Assoc 2006;42:136-146.
14. Cornell KK. Cystotomy, partial cystectomy, and tube cystotomy. Clin Tech Small Anim Pract 2000;15(1):11-16.
15. Bray JP, Doyle RS, Burton CA. Minimally invasive inguinal approach for tube cystostomy. Vet Surg 2009;38:411-416.
16. Zhang JT, Wang HB, Shi J, et al. Laparoscopy for percutaneous tube cystostomy in dogs. J Am Vet Med Assoc 2010;236(9):975-977.
17. Franz S, Dadak AM, Schoffmann G, et al. Laparoscopic-assisted implantation of a urinary catheter in male sheep. J Am Vet Med Assoc 2008;225(12):1857-1862.
18. Jones JA, Kirkpatrick AW, Hamilton DR, et al. Percutaneous bladder catheterization in microgravity. Can J Urol 2007;14(2):3493-3498.
19. Noel S, Claeys S, Hamaide A. Acquired urinary incontinence in the bitch: update and perspectives from human medicine. Part 1: the bladder component, pathophysiology and medical treatment. Vet J 2010;186:10-17.
20. Grauer, G. Disorders of micturition. In: Nelson RW, Couto GC, eds. Small animal internal medicine. 2nd ed. St. Louis, Mo: Mosby 1998;659-667.
21. Straeter-Knowlen IM, Marks SL, Rishniw M, et al. Urethral pressure response to smooth and skeletal muscle relaxants in anesthetized, adult male cats with naturally acquired urethral obstruction. Am J Vet Res 1995;56(7):919-923.
22. Lane IF, Fischer JR, Miller E, et al. Functional urethral obstruction in 3 dogs: clinical and urethral pressure profile findings. J Vet Intern Med 2000;14:43-49.
23. Gerber B, Eichenberger S, Reusch CE. Guarded long term prognosis in male cats with urethral obstruction. J Fel Med Surg 2008;10:16-23.
24. Bass M, Howard J, Gerber B, et al. Retrospective study of indications for and outcome of perineal urethrostomy in cats. J Small Anim Pract 2005;46:227-231.