Nonobstructive idiopathic feline lower urinary tract disease: How to approach a puzzling disorder
Researchers have yet to pin down the cause or causes of this frustrating and often painful disease, so a definitive treatment protocol remains elusive. Current recommendations include lifestyle changes such as stress relief and increased water intake.
Feline lower urinary tract disease (FLUTD) comprises a spectrum of clinical signs that may include pollakiuria, hematuria, stranguria, dysuria, and periuria (inappropriate urination). The urinary tract can only respond to an insult—no matter its cause—in limited ways, such as inflammation and pain, which result in the nonspecific signs listed above.
Several acronyms are used to describe the causes of lower urinary tract signs, especially those that refer to the idiopathic syndrome. FLUTD is commonly used to refer only to the idiopathic syndrome in cats. Technically, however, FLUTD encompasses all causes of lower urinary tract signs, including urolithiasis, urinary tract infection (UTI), reflex dyssynergia, trauma, congenital abnormalities, neoplasia, and sterile or idiopathic feline lower urinary tract disease (iFLUTD). Additional terms include feline urinary, or urologic, syndrome (FUS) and feline interstitial or idiopathic cystitis (FIC). Some authors contend that interstitial cystitis should be reserved for cats in which cystoscopic evidence of mucosal disruption has been confirmed.1 In this article, I use iFLUTD to emphasize that the disease entity discussed is idiopathic and LUTS (lower urinary tract signs) to refer to the nonspecific signs associated with any lower urinary tract disease.
Non-iFLUTD causes of LUTS—including urolithiasis, UTIs, neoplasia, trauma, and congenital abnormalities—must be ruled out before iFLUTD can be diagnosed. A diagnosis of iFLUTD can refer to a single episode of LUTS or chronic, recurrent clinical signs with or without urethral obstruction. Obstructive iFLUTD is life-threatening, requiring in-hospital management or surgical intervention. Detailed management of cats with obstructive iFLUTD has been described elsewhere in the literature.2,3 With either obstructive or nonobstructive iFLUTD, owners may even consider euthanasia in cases of chronic recurrent episodes because of their cats' poor quality of life and the expense and frustration of treating affected cats. In an effort to help affected cats and their owners, this article reviews the proposed causes, typical clinical signs, diagnostic testing, and medical and environmental management of cats with nonobstructive iFLUTD.
POSSIBLE CAUSES
It is important to understand the proposed causes of iFLUTD because they have led to a variety of therapies targeting those mechanisms. Many of the causes that have been suggested for iFLUTD have been extrapolated from research investigating interstitial cystitis in women. As more studies are conducted, further evidence for the cause or causes of iFLUTD may emerge, but based on the available body of knowledge, the disease appears to be multifactorial.
Infection
Bacterial cystitis leading to pain, inflammation, and LUTS is one cause to consider. Most studies investigating the general causes of LUTS report a low overall incidence (< 3%) of bacterial UTIs.1,4,5 In one large retrospective study, UTIs were identified in 12% of cats with LUTS, most of which occurred in cats > 10 years of age.6 However, a recent study evaluating cats in Norway with LUTS showed that 23% of cats with either obstructive or nonobstructive iFLUTD had positive culture results based on samples collected by either cystocentesis or midstream free-catch.7
Since most studies have been unable to demonstrate positive culture results in cats with iFLUTD, stealth organisms (those that are difficult to identify through conventional diagnostic testing) have been implicated as causative agents of iFLUTD. Ureaplasma and Mycoplasma species have been associated with UTIs in several species, including people, rodents, sheep, dogs, and cats; because they have no cell wall, these organisms are difficult to culture.8 However, in a recent study in which 91 urine samples from cats with recurrent iFLUTD and negative bacterial culture results were evaluated by using PCR assays to detect Mycoplasma and Ureaplasma species, the organisms were not identified.8 Viral particles such as bovine herpesvirus-4 and calicivirus have also been implicated.9,10 Recently, two novel feline caliciviruses were identified in two of 40 cats with iFLUTD,11 but their significance in iFLUTD is unknown.
Deficient glycosaminoglycan layer
Glycosaminoglycans are a constituent of the mucin layer that protects the urothelium and prevents urine components from coming into direct contact with the bladder mucosa. One hypothesis suggests a deficiency of the glycosaminoglycan protective layer exposes the urothelium to these components, causing tissue damage and a leaky urothelium. Tissue injury exposes and stimulates pain-sensitive fibers (C fibers), causing the release of substance P (a neurotransmitter), mast cell activation and degranulation, inflammation, and edema, which further affect the bladder urothelium, C fibers, and afferent neurons.12,13 This cascade of events, known as neurogenic inflammation, may account for the vicious cycle of pain and dysuria.
Histologic examination of bladder wall samples from cats with FIC reveals increased numbers of C fibers, mast cells, and substance P receptors.13 In addition, low rates of glycosaminoglycan excretion and increased bladder wall permeability are present in both people and cats with interstitial cystitis.14-17 There is, however, some indication that abnormalities present in people with idiopathic cystitis, such as decreased glycosaminoglycans and increased mast cells, can be present in nonidiopathic cystitis disease, suggesting that these abnormalities are not a cause but a result of idiopathic cystitis.18,19
Stress
Central nervous system involvement in the development of iFLUTD has been suggested in several studies. Areas in the brain (locus ceruleus, paraventricular nucleus) that provide excitatory input in response to bladder distention have been shown to have higher activities of an enzyme, tyrosine hydroxylase, involved in catecholamine synthesis, and significantly higher plasma catecholamine concentrations have been documented in cats with iFLUTD compared with controls.20,21 Alpha2-adrenoreceptors, which normally inhibit catecholamine release and pain input to the brain, appear to be desensitized in cats with iFLUTD, possibly because of chronically elevated catecholamine concentrations.22 Alpha2-adrenoreceptors are also found in the bladder and may play a role in blood flow.5 In these studies, cats were evaluated in both stressful and environmentally enriched conditions. Some of the parameters measured, such as catecholamine concentrations and bladder permeability, decreased during the enrichment phase.
Other evidence that suggests these cats function abnormally under stress is smaller adrenal glands and a suboptimal response to synthetic ACTH in cats with iFLUTD compared with controls.23
SIGNALMENT, HISTORY, AND PHYSICAL EXAMINATION FINDINGS
Cats with iFLUTD are typically between 4 and 7 years of age.6 No breed predisposition exists. Castrated males have an increased risk, while intact females have a decreased risk.6
Owners of cats with iFLUTD report one or more of the following signs: periuria, hematuria, pollakiuria, stranguria, or an inability to urinate.24 Cats may present in their first episode or have a chronic, recurrent history.
On physical examination, affected cats appear normal and active unless they have a urethral obstruction or are in extreme pain. It is important to assess bladder size in cats with a history of stranguria that have become depressed or obtunded or that have other systemic signs such as vomiting and anorexia. Palpation may reveal a large, turgid bladder that cannot be expressed. Steps must be taken to relieve the obstruction as quickly as possible. In contrast, the bladders of cats with nonobstructive iFLUTD are small. Even minimal palpation can result in urination because of the irritated, inflamed bladder wall. Often, no other relevant physical examination findings related to the urinary signs will be present.
CLINICAL SIGNS
The LUTS that are present with iFLUTD can be attributed to other causes (Table 1), so a thorough work-up is imperative. These possible causes of LUTS, urolithiasis in particular, should guide the work-up of cats suspected of having iFLUTD.
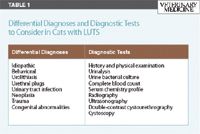
Table 1 Differential Diagnoses and Diagnostic Tests to Consider in Cats with LUTS
Periuria
Periuria is a common clinical sign, occurring in 93% of cats with iFLUTD.24 However, periuria can also be purely behavioral and should prompt questioning about the cat's environment, such as the introduction of a new cat or other pet, arrival of a new baby or household member, a recent move or change to the living environment (e.g. new carpeting, a new addition), or a change in litter or food. The roles of environment and stress in iFLUTD will be discussed later.
Hematuria
Hematuria can be caused by UTIs, urolithiasis, neoplasia, thrombocytopenia, clotting disorders, and trauma.25 UTIs are uncommon in cats < 10 years old (< 2%),5,6 but cats > 10 years of age are more likely to develop UTIs.6 Since dilute urine increases the susceptibility of animals to UTIs, concurrent illness, such as chronic renal failure, may be responsible.26,27 This age group is also more likely to have bladder tumors such as transitional cell carcinoma that can serve as a nidus of infection.6 Inherited coagulopathies are uncommon in cats.28,29 Factor XII deficiency (Hageman trait) in cats rarely results in clinical hemorrhage.
Pollakiuria and stranguria
Pollakiuria and stranguria are reported in 79% and 70% of iFLUTD cases, respectively.24 These signs can result from UTIs, urethral plugs, cystic or urethral stones, neoplasia, and iFLUTD. In one large retrospective study, urolithiasis and urethral plugs accounted for LUTS in 10% of cats, while iFLUTD accounted for 63% of cases.6 Other studies have reported ranges of 13% to 28% for urolithiasis and 55% to 69% for iFLUTD.5
DIAGNOSTIC EVALUATION
Keeping in mind that FLUTD is a constellation of diseases and that iFLUTD is a diagnosis of exclusion, each cat presenting with stranguria, pollakiuria, hematuria, periuria, or partial or complete urethral obstruction should be approached similarly. In addition to a history and physical examination, a typical work-up includes a urinalysis, urine bacterial culture, complete blood count, serum chemistry profile, and radiographic examination. Ultrasonography, double-contrast cystourethrography, and cystoscopy are included as needed. In addition, consider evaluating platelets and, in rare cases, clotting factors when hematuria is present. Clotting factor assays, such as prothrombin time and activated partial thromboplastin time, are necessary if there is evidence of bleeding elsewhere or systemic illness, such as hepatic disease or neoplasia.30
Urinalysis
Cystocentesis is preferred to obtain a urine sample but may be difficult to perform because affected cats often have small, irritated bladders. A comparison of samples obtained free-catch and by cystocentesis may be useful in cases of urethral disease. With urethral transitional cell carcinoma, for example, there may be few cytologic abnormalities in a sample obtained by cystocentesis, but transitional cells may be present in a free-catch sample. The mean urine specific gravity in cats with iFLUTD is 1.052, urine pH is usually acidic, and microscopic hematuria is present in 95% of cases.24 Pyuria may be present if inflammation is severe, but bacteriuria is uncommon.24
Urine bacterial culture
UTIs occur most commonly in cats > 10 years of age.6 Urolithiasis, neoplasia, previous urethral catheterizations, and urethrostomies also predispose cats to UTIs. A negative culture result can confirm sterile urine when pyuria caused by inflammation rather than infection is present. Interpret positive culture results from free-catch samples with caution. In cats, growth of > 10,000 CFU/ml from a midstream free-catch sample is highly suggestive of a true UTI.31 Despite the difficulty in obtaining and interpreting urine bacterial cultures, it is an important diagnostic step, given a recent study suggesting that UTIs may be more common in cats with iFLUTD than previously thought.7
Complete blood count
A complete blood count is performed to rule out other systemic illnesses since the results should be unremarkable in cats with iFLUTD.32 An inflammatory leukogram or nonregenerative anemia suggests an upper UTI, chronic kidney disease, or other inflammatory focus. Lower urinary tract inflammation alone should not cause an inflammatory leukogram. A normal platelet count excludes thrombocytopenia as a cause of the hematuria commonly present with iFLUTD.
Serum chemistry profile
Since serum chemistry profile results in cats with iFLUTD are usually unremarkable, its primary use is to rule out coexisting illness. In cats that are young and otherwise healthy, demonstrate adequate urine concentrating ability, have no abnormalities on a complete blood count, and are not obstructed, a serum chemistry profile may be unnecessary.
Radiography
Given that urolithiasis represents the second leading cause of LUTS in cats, radiography is an important initial diagnostic test to rule out radiopaque uroliths, most commonly calcium oxalate and struvite. Although the ratio of calcium oxalate uroliths to struvite uroliths increased significantly over the past 15 years, within the last three years struvite uroliths are again on the rise, representing 44% of uroliths analyzed, while the percentage of calcium oxalate uroliths dropped to 40%.33,34 Radiographic findings in cats with iFLUTD are nonspecific. Abdominal radiographs typically reveal a small bladder and no abnormalities.
Ultrasonography
Ultrasonographic examination of the urinary tract is used to identify bladder abnormalities or a tumor, assess renal architecture, rule out the more uncommon radiolucent uroliths, and obtain a urine sample when the bladder is small and irritated. Typically, bladders in cats with iFLUTD are small, which can be problematic when you are evaluating wall thickness. The bladder may contain sludge—small hyperechoic particles that represent white blood cells and crystals that precipitate because of the highly concentrated urine. The distal urethra cannot be visualized ultrasonographically.31
Double-contrast cystourethrography
Double-contrast cystourethrography is the radiographic imaging modality of choice to evaluate bladder wall thickness, mucosal margins, and filling defects and to assess the urethra. This diagnostic tool is particularly valuable in ruling out uroliths, neoplasia, congenital anomalies, and urethral disease as causes of a cat's LUTS. Double-contrast radiographic studies are most appropriate in cases of recurrent iFLUTD.5
Cystoscopy
Cystoscopy is indicated when urethral disease or urethral or bladder neoplasia is suspected, for laser access to fragment urethral calculi, and to support a diagnosis of iFLUTD. The presence of pinpoint hemorrhages called glomerulations, a term borrowed from the literature on interstitial cystitis in women, is consistent with a diagnosis of iFLUTD.13
Cystoscopy is becoming more available in private practice, especially in dogs. However, the size of the endoscopes required (1.9-mm rigid arthroscope for female cats; 1.2-mm flexible cystourethroscope for males) may make cystoscopy of the feline urinary tract less possible than other endoscopic procedures such as gastrointestinal endoscopy and rhinoscopy.35 Fortunately, cystoscopy is not required to make a presumptive diagnosis of iFLUTD if other diseases are ruled out and LUTS are present.
Diagnostic overview
Using the diagnostic tests recommended above, you can rule out most other causes of LUTS and presumptively diagnose iFLUTD. For healthy cats with first-time occurrences, a urinalysis, urine bacterial culture, and plain abdominal radiographic examination are the minimum diagnostic tests that should be performed. For cats with chronic, recurrent LUTS, a complete blood count, a serum chemistry profile, more advanced imaging such as double-contrast urethrography and ultrasonography, and special procedures (cystoscopy) are warranted.
REVIEW OF THERAPIES
The difficulty of evaluating the efficacy of therapies for iFLUTD is that this disease is self-limiting, resolving within five to 10 days regardless of the therapy used.36 Various therapies addressing each proposed mechanism of action have been investigated, usually in retrospective studies in which many confounding variables had to be considered or in small prospective studies that were not blinded or that did not use controls (Table 2).
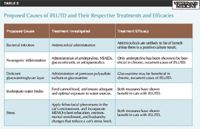
Table 2 Proposed Causes of iFLUTD and Their Respective Treatments and Efficacies
Address infections
Theory. Infectious agents, including stealth organisms, are responsible for iFLUTD.
Evidence. Most studies, including those investigating interstitial cystitis in women, indicate little evidence to support an infectious cause of iFLUTD.1,4,6,8 Despite recent reports of increased percentages of UTIs and the identification of novel feline caliciviruses with iFLUTD, further investigation is needed before antimicrobials or antivirals can be recommended (see the discussion regarding causes of iFLUTD).
Bottom line. Do not administer antimicrobials unless the urine bacterial culture results are positive.
Alleviate pain and inflammation
Theory. Pain and inflammation are due to neurogenic stimulation and increases in mast cells and substance P.
Evidence. The efficacy of amitriptyline, nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, and antispasmodics in cats with iFLUTD has been investigated.
- Amitriptyline (2.5 to 10 mg/cat/day given orally37 ): This tricyclic antidepressant is an anticholinergic, antihistamine, anti-alpha-adrenergic, anti-inflammatory, and analgesic. In one study, nine of 15 cats with chronic iFLUTD had decreased clinical signs after amitriptyline administration for 12 months.36 However, in another study in which cats with iFLUTD received either a placebo or amitriptyline for seven days, no differences in clinical signs between the two groups were found.38 This finding was also confirmed in a separate study of short-term amitriptyline use.39 The disappointing results in these studies may have been due to the short-term drug administration. Amitriptyline can cause somnolence, decreased grooming, and weight gain.36
- NSAIDS: Piroxicam and meloxicam have been used in cats with LUTS with some anecdotal success, but no controlled prospective studies have been performed.5,40 Before using any NSAID, make sure the patient's hydration status and renal function are adequate. I cannot make recommendations about their safe and effective use in cats with iFLUTD because controlled studies are lacking.
- Glucocorticoids: A double-blind clinical study in cats with iFLUTD showed no difference in clinical signs or recurrence in control cats vs. those receiving glucocorticoids.41 Thus, glucocorticoid administration is not recommended, especially if NSAIDs are being administered concurrently.
- Antispasmodics (e.g. diazepam, dantrolene, phenoxybenzamine, propantheline, acepromazine): Limited studies in cats with iFLUTD have shown some relief with a few of these drugs in the treatment of urethral smooth muscle and skeletal muscle spasms. Because of possible side effects and a lack of studies in cats with iFLUTD for each drug, no single agent can be recommended.5,40
Bottom line. Amitriptyline may be useful when given long-term in chronic, recurrent cases but is not helpful in acute episodes.
Supplement glycosaminoglycans
Theory. The glycosaminoglycan layer is deficient, allowing for toxic insult to the urothelium.
Evidence. Pentosan polysulfate sodium and glucosamine are two agents that have been studied in cats with iFLUTD.
- Pentosan polysulfate sodium (2 to 16 mg/kg b.i.d. or 8 mg/kg b.i.d. given orally42 ): This particular glycosaminoglycan has been shown to be helpful in 28% to 68% of people with idiopathic cystitis and has been used anecdotally in some cats with success.43 Elmiron (Ortho-McNeil-Janssen Pharmaceuticals), the product approved in the United States for use in people, needs to be formulated to smaller capsule sizes. The drug is well-tolerated in cats, and though it can cause bleeding in any species because of its anticoagulant properties, this side effect has not specifically been reported in cats.42
- Glucosamine (Cosequin for Cats—Nutramax Laboratories) (1 capsule [125 mg glucosamine, 100 mg chondroitin sulfate] daily for cats < 10 lb; 1 capsule b.i.d. for cats > 10 lb given orally44 ): One study showed no significant difference between the severity or duration of iFLUTD in client-owned cats receiving oral glucosamine vs. a placebo. Two cats in the placebo group, however, were euthanized because of severe, recurrent disease.43 Side effects can include minor gastrointestinal signs such as flatulence and soft stool.44
Bottom line. Oral glucosamine supplementation has few side effects, and long-term therapy may be useful in conjunction with other therapies in cats with chronic, recurrent iFLUTD.
Increase water intake
Theory. A decreased urine concentration decreases the concentration of components that may be toxic to the urothelium.
Evidence. Dilute urine may reduce the concentration of noxious urinary components that can be bladder wall irritants.12,43,45 Several studies evaluating dietary or other supplements in the treatment of iFLUTD in cats concluded that the main correlation between improvement in clinical signs or reduced recurrences was the feeding of a canned diet.43,46 Offer cats canned food choices, and then remove the dry food gradually. This measure establishes a constancy of the water content and diet composition, which appears to be important.5 Drinking water preferences, such as bowl type, water depth, and running vs. still water, should be determined to ensure adequate water intake.
Bottom line. Transition to a consistent canned diet, and encourage water consumption by determining a cat's drinking preferences.
Alleviate stress
Theory. Stress has been associated with iFLUTD recurrence and may play a role in the disease's pathophysiology, both systemically and locally in the bladder.
Evidence. Stress reduction measures that have been investigated in cats with iFLUTD include feline facial pheromones and environmental modification.
- Pheromones, chemical substances that are found, for example, in sebaceous secretions in the cheeks, likely affect the limbic and hypothalamic regions.47,48 The F3 fraction of the five facial pheromone fractions isolated in cats is deposited on objects by facial rubbing and serves to mark territory and decrease aggressive behavior. Feliway (Ceva Santé Animale), a synthetic analogue of the F3 fraction of feline facial pheromone, has been used for behavior modification, including urine spraying.47 In a clinical study, Feliway resulted in a trend (though no statistically significant difference was noted) toward fewer days of clinical signs of cystitis and a reduced number of episodes of iFLUTD.49
- Multimodal environmental modification: Implementation of a stress and environmental management protocol that uses client education, environmental enrichment, and husbandry changes appears to be an important aspect of therapy. Multimodal environmental modification (MEMO) involves making adjustments to litter boxes (number, location, size and shape, litter type), scratching posts (number, location, texture), sleeping and eating areas, perches, and toys.5,48,50 Client education includes providing information about cat behavior in relation to people and other cats, explaining the iFLUTD syndrome, empathizing with the owner's frustrations and concerns, and encouraging the owner not to blame the cat for the disorder.50 Tailor MEMO to the specific surroundings and interactions in a cat's environment. A recent study in which owners used MEMO demonstrated a significant reduction in their cats' LUTS, fear, nervousness, and respiratory signs (coughing, sneezing, wheezing) and a trend toward reduced aggression. In 70% to 75% of the 46 cats in this study, there was no evidence of LUTS in the 10-month follow-up period.50
Bottom line. Incorporate MEMO in the management of iFLUTD, and add synthetic feline facial pheromones as a component of stress management. For more information, see The Indoor Cat Initiative through The Ohio State University College of Veterinary Medicine Web site: http://www.vet.ohio-state.edu/indoorcat.
THERAPEUTIC RECOMMENDATIONS
Based on the current literature, the most important therapies appear to be stress management using feline facial pheromones and MEMO and increasing water intake through the use of canned diets. No specific canned diet is recommended but rather is determined by the cat's preference. For chronic recurrent episodes, adjunctive therapy with long-term amitriptyline and glycosaminoglycan supplementation may be beneficial.
SUMMARY
A frustrating and potentially life-threatening disease in cats, iFLUTD results in pain, pollakiuria, hematuria, periuria, stranguria, and, in some cases, urethral obstruction. It is a diagnosis of exclusion made only after conducting a thorough work-up. The results of studies evaluating possible causes have been conflicting and reveal that the syndrome is likely multifactorial. Further studies are needed to establish the contributions of each possible mechanism.
The efficacy of specific treatments is difficult to assess because of iFLUTD's self-limiting nature. In general, drug therapies that attempt to target potential causes have had disappointing results. The management tactics that seem most promising include reducing stress through MEMO and feline facial pheromones and adjusting the diet to include canned food and increased water intake. Amitriptyline and glycosaminoglycan supplementation may provide additional benefits for chronic, recurrent episodes, but further studies are needed to establish efficacy.
Kristy Dowers, DVM, MS, DACVIM
Department of Clinical Sciences
College of Veterinary Medicine and Biomedical Sciences
Colorado State University
Fort Collins, CO 80523
REFERENCES
1. Buffington CAT, Chew DJ, Kendall MS, et al. Clinical evaluation of cats with nonobstructive urinary tract diseases. J Am Vet Med Assoc 1997;210(1):46-50.
2. Osborne CA, Kruger JM, Lulich JP, et al. Feline lower urinary tract diseases. In: Ettinger SJ, Feldman EC, eds. Textbook of veterinary internal medicine. 5th ed. Philadelphia, Pa: WB Saunders Co, 2000;1734-1737.
3. Osborne CA, Lees GE, Polzin DJ, et al. Immediate relief of feline urethral obstruction. Vet Clin North Am Small Anim Pract 1984;14(3):585-597.
4. Kruger JM, Osborne CA, Goyal SM, et al. Clinical evaluation of cats with lower urinary tract disease. J Am Vet Med Assoc 1991;199(2):211-216.
5. Hostutler RA, Chew DJ, DiBartola SP. Recent concepts in feline lower urinary tract disease. Vet Clin North Am Small Anim Pract 2005;35(1):147-170.
6. Lekcharoensuk C, Osborne CA, Lulich JP. Epidemiologic study of risk factors for lower urinary tract diseases in cats. J Am Vet Med Assoc 2001;218(9):1429-1435.
7. Eggertsdöttir AV, Lund HS, Krontveit R, et al. Bacteriuria in cats with feline lower urinary tract disease: a clinical study of 134 cases in Norway. J Feline Med Surg 2007;9(6):458-465.
8. Abou N, Houwers DJ, van Dongen AM. PCR-based detection reveals no causative role for Mycoplasma and Ureaplasma in feline lower urinary tract disease [Letter to the editor]. Vet Microbiol 2006;116(1-3):246-247.
9. Fabricant CG. The feline urologic syndrome induced by infection with a cell-associated herpesvirus. Vet Clin North Am Small Anim Pract 1984;14(3):493-502.
10. Kalkstein TS, Kruger JM, Osborne CA. Feline idiopathic lower urinary tract disease. Part II. Potential causes. Compend Contin Educ Pract Vet 1999;21(2):148-154.
11. Rice CC, Kruger JM, Venta PJ, et al. Genetic characterization of 2 novel feline caliciviruses isolated from cats with idiopathic lower urinary tract disease. J Vet Intern Med 2002;16(3):293-302.
12. Gunn-Moore DA. Proceedings of the ESFM Feline Congress (Stockholm, 2002): feline lower urinary tract disease. J Feline Med Surg 2003;5(2):133-138.
13. Buffington CAT, Chew DJ, Woodworth BE. Feline interstitial cystitis. J Am Vet Med Assoc 1999;215(5):682-687.
14. Metts JF. Interstitial cystitis: urgency and frequency syndrome. Am Fam Physician 2001;64(7):1199-1206.
15. Pereira DA, Aguiar JAK, Hagiwara MK, et al. Changes in cat urinary glycosaminoglycans with age and in feline urologic syndrome. Biochem Biophys Acta 2004;1672(1):1-11.
16. Lavelle JP, Meyers SA, Ruiz WG, et al. Urothelial pathophysiological changes in feline interstitial cystitis: a human model. Am J Physiol Renal Physiol 2000;278(4):F540-F553.
17. Buffington CAT, Blaisdell JL, Binns SP Jr, et al. Decreased urine glycosaminoglycan excretion in cats with interstitial cystitis. J Urol 1996;155(5):1801-1804.
18. Elbadawi A. Interstitial cystitis: a critique of current concepts with a new proposal for pathologic diagnosis and pathogenesis. Urology 1997;49(5A Suppl):14-40.
19. Erickson DR. Interstitial cystitis: update on etiologies and therapeutic options. J Womens Health Gend Based Med 1999;8(6):745-758.
20. Reche Júnior A, Buffington CAT. Increased tyrosine hydroxylase immunoreactivity in the locus coeruleus of cats with interstitial cystitis. J Urol 1998;159(3):1045-1048.
21. Westropp JL, Kass PH, Buffington CAT. Evaluation of the effects of stress in cats with idiopathic cystitis. Am J Vet Res 2006;67(4):731-736.
22. Westropp JL, Kass PH, Buffington CAT. In vivo evaluation of alpha2-adrenoreceptors in cats with idiopathic cystitis. Am J Vet Res 2007;68(2):203-207.
23. Westropp JL, Welk KA, Buffington CAT. Small adrenal glands in cats with feline interstitial cystitis. J Urol 2003;170:2494-2497.
24. Kalkstein TS, Kruger JM, Osborne CA. Feline idiopathic lower urinary tract disease. Part I. Clinical manifestations. Compend Contin Educ Pract Vet 1999;21(1):15-26.
25. Forrester SD. Diagnostic approach to hematuria in dogs and cats. Vet Clin North Am Small Anim Pract 2004;34(4):849-866.
26. Bartges JW. Urinary tract infections. In: Ettinger SJ, Feldman EC, eds. Textbook of veterinary internal medicine. 6th ed. St. Louis, Mo: Elsevier Saunders Co, 2005;1800-1808.
27. Lees GE. Bacterial urinary tract infections. Vet Clin North Am Small Anim Pract 1996;26(2):297-304.
28. Carr AP. Inherited coagulopathies. In: Ettinger SJ, Feldman EC, eds. Textbook of veterinary internal medicine. 6th ed. St. Louis, Mo: Elsevier Saunders, 2005;1929-1933.
29. Peterson JL, Couto CG, Wellman ML. Hemostatic disorders in cats: a retrospective study and review of the literature. J Vet Intern Med 1994;9(5):298-303.
30. Brooks MJ, Catalfamo JL. Platelet disorders and von Willebrand disease. In: Ettinger SJ, Feldman EC, eds. Textbook of veterinary internal medicine. 6th ed. St. Louis, Mo: Elsevier Saunders, 2005;1918-1929.
31. Bartges JW. Diagnosis of urinary tract infections. Vet Clin North Am Small Anim Pract 2004;34(4):923-933.
32. Kalkstein TS, Kruger JM, Osborne CA. Feline idiopathic lower urinary tract disease. Part III. Diagnosis. Compend Contin Educ Pract Vet 1999;21(5):387-394.
33. Cannon AB, Westropp JL, Ruby AL, et al. Evaluation of trends in urolith composition in cats: 5,230 cases (1985-2004). J Am Vet Med Assoc 2007;231(4):570-576.
34. Lekcharoensuk C, Lulich JP, Osborne CA, et al. Association between patient-related factors and risk of calcium oxalate and magnesium ammonium phosphate urolithiasis in cats. J Am Vet Med Assoc 2000;217(4):520-525.
35. Chew DJ, Buffington CAT, Kendall MS, et al. Urethroscopy, cystoscopy, and biopsy of the feline lower urinary tract. Vet Clin North Am Small Anim Pract 1996;26(3):441-462.
36. Chew DJ, Buffington CAT, Kendall MS, et al. Amitriptyline treatment for severe recurrent idiopathic cystitis in cats. J Am Vet Med Assoc 1998;213(9):1282-1286.
37. Plumb DC. Amitriptyline. In: Plumb's veterinary drug handbook. 5th ed. Stockholm, Wis: PharmaVet Inc;2005;35-37.
38. Kraijer M, Fink-Gremmels J, Nickel RF. The short-term clinical efficacy of amitriptyline in the management of idiopathic feline lower urinary tract disease: a controlled clinical study. J Feline Med Surg 2003;5(3):191-196.
39. Kruger JM, Conway TS, Kaneene JB, et al. Randomized controlled trial of the efficacy of short-term amitriptyline administration for treatment of acute, nonobstructive, idiopathic lower urinary tract disease in cats. J Am Vet Med Assoc 2003;222(6):749–758.
40. Kalkstein TS, Kruger JM, Osborne CA. Feline idiopathic lower urinary tract disease. Part IV. Therapeutic options. Compend Contin Educ Pract Vet 1999;21(6):497-509.
41. Osborne CA, Kruger JM, Lulich JP, et al. Prednisone therapy of idiopathic feline lower urinary tract disease: a double-blind clinical study. Vet Clin North Am Small Anim Pract 1996;26(3):563-569.
42. Plumb DC. Pentosan polysulfate sodium. In: Plumb's veterinary drug handbook. 6th ed. Stockholm. Wis.: PharmaVet Inc, 2008;712-713.
43. Gunn-Moore DA, Shenoy CM. Oral glucosamine and the management of feline idiopathic cystitis. J Feline Med Surg 2004;6(4):219-225.
44. Plumb DC. Glucosamine. In: Plumb's veterinary drug handbook. 6th ed. Stockholm. Wis.: PharmaVet Inc, 2008;429-431.
45. Houston DM, Moore AEP, Favrin MG, et al. Feline urethral plugs and bladder uroliths: a review of 5484 submissions 1998-2003. Can Vet J 2003;44(12):974-977.
46. Markwell PJ, Buffington CAT, Chew DJ, et al. Clinical evaluation of commercially available urinary acidification diets in the management of idiopathic cystitis in cats. J Am Vet Med Assoc 1999;214(3):361-365.
47. Pageat P, Gaultier E. Current research in canine and feline pheromones. Vet Clin North Am Small Anim Pract 2003;33(2):187-211.
48. Westropp JL, Buffington CAT. Feline idiopathic cystitis: current understanding of pathophysiology and management. Vet Clin North Am Small Anim Pract 2004;34(4):1043-1055.
49. Gunn-Moore DA, Cameron ME. A pilot study using feline facial pheromone for the management of feline idiopathic cystitis. J Feline Med Surg 2004;6(3):133-138.
50. Buffington CAT, Westropp JL, Chew DJ, et al. Clinical evaluation of multimodal environmental modification (MEMO) in the management of cats with idiopathic cystitis. J Feline Med Surg 2006;8(4):261-268.