Not one good leg to stand on ... literally
What a bear of a dog taught this veterinary technician about bad luck, teamwork and the strength of the human-animal bond.

Despite multiple surgeries, physical therapy and rehabiliation, Bubba's limbs were unable to carry him.
The story of Bubba, the biggest and most lovable Newfie anyone could meet, began in July 2017 at the University of Tennessee Veterinary Medical Center (UTVMC) when his owner contacted our orthopedic service about treating Bubba's hip dysplasia with bilateral total hip replacement (THR). The 2-year-old, 156-lb, castrated Newfoundland would be traveling to us from Wisconsin, so coordinating his first appointment for a full evaluation, including any necessary testing and imaging, was important.
We couldn't have guessed how many times over the next year Bubba's owner would drive his dog the 10+ hours to and from our hospital.
Bubba's story
In addition to hip dysplasia, Bubba's clinical history included bilateral fragmented medial coronoid process, which had been treated about a year earlier at the University of Wisconsin's veterinary hospital with bilateral elbow arthroscopy. Our initial orthopedic examination on July 3, 2017 revealed bilateral hip dysplasia as well as osteoarthritis that resulted from the dog's fragmented medial coronoid process.
Radiographs confirmed severe subluxation and osteoarthritis, with the most advanced changes present in the left hip. Cranial luxation of the femoral head was noted bilaterally, corresponding with Bubba's clinical signs of pain, reduced range of motion and muscle atrophy on the left side (Figure 1)

Figure 1A

Figure 1B
Figure 1. Ventrodorsal (A) and left lateral (B) radiographic views of Bubba's pelvis showed cranial luxation of the femoral head. (All radiographic images courtesy of UTVMC's radiology service.)
A left THR was performed about six weeks later, on August 15, 2017. Postoperative radiographs showed that the femoral stem on the left side wasn't centralized in the canal; instead it was angled such that the tip of the stem contacted the cortex of the femur. Bubba was taken back to surgery later that day, where the original #7 stem was replaced with a #8 stem. To facilitate placement of the larger stem, the femoral neck was cut shorter (i.e., lower on the femur). The new stem was placed more centrally in the femur, but now the prosthetic hip luxated ventrally due to the shortening of the femoral neck. The +0 femoral head was replaced with a 6+ head-increasing the femoral neck length and thus stabilizing the hip-then the femoral head was reduced (Figure 2). Discharge instructions for Bubba included strict activity restriction for eight to 12 weeks.

Figure 2A
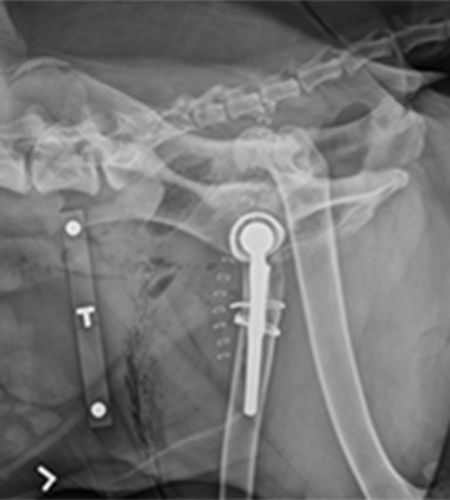
Figure 2B
Figure 2. Ventrodorsal (A) and left lateral (B) radiographic views of the pelvis following Bubba's third surgery in which the femoral neck was shortened and a larger femoral stem and head were placed. Note that the stem on the left side isn't centralized in the canal; instead it is angled such that the tip of the stem touches the femoral cortex.
At Bubba's 2-week postsurgical recheck, hobbles were applied to help prevent hindlimb splaying and caudoventral luxation, and Bubba was fitted with a Help ‘Em Up harness. At the 6-week recheck on September 25, 2017, the implants were still in the proper position, but Bubba's hindlimbs remained weak with limited range of motion. Continued activity restriction was advised at that time.
By 11 weeks post surgery, Bubba's muscle atrophy had progressed and physical rehabilitation was recommended to help him build muscle strength. About a week later, the dog presented to our emergency and critical care service for craniodorsal luxation of his left THR. It was unclear whether the additional physical therapy played a role or if a separate event led to the dislocation. Bubba was transferred to the orthopedic service where a closed hip reduction was performed under fluoroscopic guidance. He was then placed in an Ehmer sling, with plans for recheck radiographs and potential sling removal in 1 week. Unfortunately, the hip was luxated at that recheck, and the owner elected explantation of the THR components, which was performed at our hospital.
Four months later, during a recheck by his primary veterinarian, Bubba was doing well, with the left hip functioning normally following femoral head and neck osteotomy. However, he was presented to our emergency and critical care service shortly thereafter for right hindlimb lameness. Bubba's primary veterinarian had diagnosed a cranial cruciate ligament rupture after the dog slipped and fell in a creek, and radiographs were taken for measurement of the tibial plateau angle in preparation for tibial plateau leveling osteotomy (TPLO). On the day of his surgery we noted superficial pyoderma, so the procedure was postponed and Bubba was placed on antibiotics with a plan for him to return in 3 weeks. On March 27, 2018 a right TPLO was performed. Postoperative posteroanterior radiographs revealed medial patella luxation. Bubba likely had patellar instability that worsened following the cranial cruciate ligament rupture, and the posteroanterior positioning for radiography put further pressure on the patella, luxating it.
On March 29, 2018, Bubba underwent surgical repair of the luxation at UTVMC via a right lateral fabellar-tibial suture. A lateral imbrication of the synovium was performed, and the sutures in the fibrous capsule that had been placed previously to close the medial arthrotomy were removed. This allowed the tissues to loosen medially and tighten laterally, reducing the medial tension on the patella. Bubba remained hospitalized for the next several weeks. On the day of his discharge, May 7, 2018, his TPLO was healing (indicated by smooth cortical margins at the osteotomy site on radiographs) and Bubba was able to ambulate with very little assistance.
On June 12, 2018, Bubba presented for his 9-week recheck, at which time we noted that the TPLO was healing but his patella had re-luxated. The owner was offered four surgical options for Bubba: (1) distal femoral osteotomy to correct angulation of the femur, (2) tibial tuberosity transposition, (3) patellar groove prosthesis or (4) patellectomy. The owner left it to the surgeon to decide what would be most successful for Bubba as this would be the last surgery he would put his dog through. Tibial tuberosity transposition, medial and lateral imbrication of the joint capsule, and trochleoplasty (a procedure to deepen the groove) were performed that day (Figure 3). Bubba stayed in the hospital's physical therapy and rehabilitation service for the next three weeks.

Figure 3A

Figure 3. Postoperative lateral (A) and right posteroanterior (B) radiographs show the right stifle following tibial tuberosity transposition, medial and lateral imbrication of the joint capsule, and trochleoplasty.
Bubba did well until July 30, 2018, when we received a call from his owner stating that Bubba couldn't stand on his right hindlimb. After consultation with the orthopedic and physical therapy service clinicians, the owner elected to take Bubba to his regular veterinarian. Re-luxation of the right patella was noted on examination, and the owner was presented with three treatment options: (1) distal femoral osteotomy, (2) patellar groove prosthesis or (3) patellectomy. Believing it was not in his dog's best interest to pursue additional surgery, the owner elected to have Bubba euthanized.
What Bubba taught me
Newfoundlands have an average life span of eight to nine years. They are prone to hereditary and congenital diseases such as hip dysplasia, fragmented coronoid process, cranial cruciate ligament rupture and medial patella luxation, all of which Bubba had. They are also predisposed to osteochondritis dissecans of the shoulder and stifle. Bubba's owner was very aggressive in pursuing treatment options to try to make his dog as comfortable as possible. Nevertheless, complications resulting in poor quality of life led to the decision for euthanasia.
Despite being young-and thus statistically less likely to have so many musculoskeletal problems-Bubba's many maladies led to significant loss of strength, coordination and function. Although veterinary orthopedic procedures generally have a high success rate, complications increase when multiple procedures are performed on multiple legs in the same dog. Some animals have constitutional orthopedic disorders that affect limb function and the individual's ability to compensate. In Bubba's case, all four limbs eventually succumbed to major orthopedic abnormalities requiring major corrective surgeries.
The overall goal of orthopedic surgery is to decrease pain and increase function, and success depends in part on the patient's ability to recover well. That's why care for the seriously affected individual must be devised for maximum benefit, which means a team approach with a combined effort from specialists in pain management, physical rehabilitation, nutrition, orthopedics and so on.
More clearly defined methods of risk assessment should be developed to guide the veterinarian in deciding what procedures in what sequence would increase the chances for such a profoundly affected animal to survive.
Breed-dependent risk assessments and physical rehabilitation endpoints must be established for these types of cases. With regard to surgical expectations and outcomes, the veterinary team must consider the limitations of each procedure, the owner's frustrations as well as the patient's quality of life.
Bubba's recovery was compromised due to his poor muscle strength, multiple limb problems, large size and laidback personality. In the final analysis of this case, Bubba truly ended up without a leg to stand on, but his experience will help move us all to a higher level of care for such difficult cases.
Jessica Montoya has been working in veterinary medicine for 15 years. For the past four years she has been a senior technician 1 at the University of Tennessee College of Veterinary Medicine. Jessica loves orthopedics and plans to pursue veterinary technician specialty certification in surgery.
Acknowledgment
The author would like to thank Joseph Weigel, DVM, MS, DACVS; Darryl Millis, DVM, MS, DACVS, CCRP, DACVSMR; and UTVMC's radiology and orthopedic services for their assistance with this case report.
