Screening and medical management of feline kidney transplant candidates
Kidney transplantation is indicated in cats with decompensated chronic kidney disease or, less commonly, acute, irreversible renal failure.
Kidney transplantation is a viable therapeutic alternative for cats with end-stage renal failure. The first successful kidney transplantation in a cat was performed in 1987 at the University of California-Davis School of Veterinary Medicine.1 Veterinary surgeons at transplant centers across the country have since performed several hundred successful kidney allograft transplants in cats.
Not all patients with chronic kidney disease are good candidates for kidney transplantation, and postoperative care requires intense medical management. In this article, we review the indications, diagnostic evaluation, and complications of kidney transplantation in cats. We also briefly describe the medical and surgical management of these patients.
CHRONIC KIDNEY DISEASE: A COMMON CAUSE OF MORBIDITY AND MORTALITY
Chronic kidney disease is a progressive, irreversible condition that affects a large percentage of cats. It is among the most common diseases in older cats, with a reported prevalence of 1.6% to 20%.2,3 One study reported the prevalence of renal failure was 12% in all cats examined at a referral-based veterinary teaching hospital.4 In geriatric cats older than 15 years, the prevalence increased to slightly greater than 30%.
Chronic kidney disease is characterized by functional or structural injury that has resulted in irreversible histologic changes. Kidney function is evaluated by performing a complete blood count, a serum chemistry profile, a urinalysis, and diagnostic imaging. Changes in blood urea nitrogen and creatinine concentrations and possible abnormalities in serum phosphorus concentrations, other electrolyte concentrations, and hematocrit or packed cell volume (PCV) combined with decreased urine concentrating ability are commonly used to assess the severity and progression of disease.
Fortunately, the kidneys have a tremendous reserve capacity; however, this reserve can delay the diagnosis of acute or chronic kidney disease until marked damage has occurred. Inadequate urine concentrating ability is generally associated with a loss of two-thirds of functional nephrons, while a loss of three-fourths of functional nephrons results in azotemia. Cats may maintain some concentrating ability despite azotemia and, thus, may be in overt renal failure without isosthenuria. By the time renal dysfunction is detected by using standard clinicopathologic tests, clinicians must assume that kidney disease is severe. In some cats, kidney transplantation offers successful treatment.
HISTORY OF KIDNEY TRANSPLANTS
Organ transplantation was first attempted early in the 20th century, using animal models. Kidney allograft transplantation (organs from other individuals of the same species) was first described by Alexis Carrel, who pioneered many vascular surgical techniques still used today.5 Early transplants were technically successful, although the transplanted kidney allografts were inevitably rejected. It was not until the development of immunosuppressive drugs in the early 1960s that prolonged survival was achieved.6 Cyclosporine revolutionized kidney transplantation through its selective inhibition of T lymphocytes, the main cell type responsible for kidney allograft rejection.7,8
Kidney transplantation is the treatment of choice in many people with end-stage kidney disease. It is an attractive alternative to hemodialysis or long-term peritoneal dialysis since quality of life and survival are greater. The transplant patient mortality rate is less than 5% in the first year.9 This success rate is a reflection of extensive research in immunosuppressive therapy and recipient-donor matching. Live donor allografts remain superior to cadaveric grafts, but 60% of patients still receive grafts from human cadavers because of insufficient donor numbers.9
Over the last decade, organ transplantation in veterinary medicine has become more common. Corneal, bone marrow, and kidney grafts have all been successfully transplanted. Kidney allograft transplantation has been successful in both dogs and cats, although canine kidney transplantation presents a greater challenge because of the level of immunosuppression required to prevent allograft rejection.10,11 Rejection episodes in dogs are frequent and severe, and canine recipients require multiple-agent immunosuppressive protocols and intensive management.10,12 Several recent studies have explored triple-drug (cyclosporine, azathioprine, and prednisolone) protocols and histocompatibility matching with limited success; to date, high complication and mortality rates in dogs still preclude widespread use of kidney transplantation.12
However, kidney allograft transplantation in cats has become an accepted treatment for patients with end-stage kidney disease. In a study of 66 cats receiving kidney transplants at the University of California-Davis School of Veterinary Medicine, 71% of the cats survived until discharge.13 The one-year survival rate in this early case series was 51%, but advances in surgical technique have anecdotally resulted in greater survival times.14,15
INDICATIONS
Kidney transplantation is indicated in cats with decompensated chronic kidney disease or, less commonly, acute, irreversible renal failure. The critical first step for ensuring a successful outcome is appropriate patient selection. Cats whose renal function continues to decompensate despite aggressive medical management are candidates for kidney transplantation.
The most common pathologic conditions for which kidney transplantation is performed include chronic interstitial nephritis (48%), polycystic kidneys (10%), ethylene glycol toxicosis (9%), and renal fibrosis (6%).13 However, transplants have also been performed in cats with advanced kidney disease due to glomerulonephritis, pyelonephritis, amyloidosis, oxalate nephrosis, renal dysplasia, pyogranulomatous nephritis, or nephrosclerosis secondary to drug toxicosis.14,16
MEDICAL MANAGEMENT OF CHRONIC KIDNEY DISEASE
Medically managing cats with chronic kidney disease begins by identifying the underlying cause of kidney dysfunction. In a study of kidney biopsy findings in cats with chronic kidney disease, tubulointerstitial nephritis was observed in 70% of cats, glomerulonephropathy in 15%, and lymphoma in 11%.17 But keep in mind that both tubulointerstitial nephritis and glomerulonephropathy are histologic rather than etiologic diagnoses. Serial assessment of any cat with chronic kidney disease is required to tailor therapy and provide prognostic information. Direct therapy at slowing the progression of disease through supportive and symptomatic therapy.
The cornerstone of patient management is a combination of dietary and drug therapy, which minimizes the clinical and physiologic consequences of reduced renal function.
Provide the right diet
Dietary recommendations vary based on the International Renal Interest Society (IRIS) stage of disease, but once azotemia is present, a diet formulated for kidney disease management is recommended.18 A delicate balance exists between reducing protein intake and maintaining appetite and body weight. It is important for cats with mild to moderate chronic kidney disease to maintain adequate caloric intake to avoid protein malnutrition. Protein, phosphorus, and sodium restriction should begin when azotemia persists in the well-hydrated state (IRIS stage 2 disease).18 Proteinuric cats may benefit from treatment with an angiotensin-converting enzyme inhibitor such as benazepril, although a definitive benefit is still lacking.19,20
Ensure adequate hydration
Adequate hydration is equally important for maintaining renal function. Polyuric, uremic cats are prone to dehydration, which contributes to progressive renal dysfunction. Strategies to improve water consumption include providing fresh water, using drinking fountains, and feeding a canned food diet. Subcutaneous fluid administration may be indicated with progression of renal insufficiency or uremia since fluid administration may help maintain optimal hydration and improve the quality of life for many cats.
Treat anemia
Anemia develops in later stages of chronic kidney disease as a multifactorial consequence of decreased erythropoietin production by the failing kidneys, decreased erythrocyte survival due to uremic toxins, and gastrointestinal bleeding. Recombinant human erythropoietin administration is effective in correcting nonregenerative anemia in most cats with chronic kidney disease.21 Many treated cats demonstrate an improvement in appetite and quality of life, although the risks of anti-erythropoietin antibody formation, polycythemia, and hypertension require careful monitoring.
Address other consequences of renal damage
Ongoing causes and consequences of renal injury that should be addressed include hypertension, uremic gastritis, metabolic acidosis, and mineral and electrolyte abnormalities such as hypokalemia, hyperphosphatemia, and hypercalcemia.
Hypertension is a well-documented sequela of chronic kidney disease, with a recently reported prevalence of 20% in affected cats.22 Evaluate cats with consistently elevated systolic blood pressure readings for ocular manifestations of hypertensive retinopathy, including retinal hemorrhages, retinal detachment, and blindness. Amlodipine, a calcium channel blocker, is effective in managing hypertension and reducing the prevalence of ocular lesions in cats.23-25
Uremic gastritis presumptively develops because of reduced clearance of plasma gastrin. The degree of hypergastrinemia may be an indicator of the severity of chronic kidney disease.26 H2-receptor blocking agents, such as famotidine, are commonly used to improve appetite and nutritional intake, presumptively through decreased severity of gastrointestinal ulceration.
Metabolic acidosis in people can exacerbate azotemia and promote further protein catabolism, muscle wasting, and hypokalemia.27 Alkalization therapy (usually oral potassium citrate or sodium bicarbonate) is indicated if acidosis is severe; commercial renal diets are formulated with alkalizers.
Hypokalemia (reported in 20% to 30% of cats with chronic kidney disease) may exacerbate kidney disease and can cause weakness and muscle wasting.28 Provide supplementation with oral potassium gluconate or potassium citrate in these cats.
Hyperphosphatemia develops secondary to a decreased glomerular filtration rate. Oral phosphate-binding agents are indicated in cats that cannot maintain normal serum phosphorus concentrations with dietary phosphorus restriction alone.

Table 1 Initial Diagnostic Evaluation of Feline Kidney Transplant Candidates
Calcitriol production may also be impaired in chronic kidney disease, disrupting calcium homeostasis and contributing to the development of renal secondary hyperparathyroidism.29 Calcitriol supplementation is now advocated in dogs with normal phosphorus and increased serum parathyroid hormone (PTH) concentrations.30 Monitor serum phosphorus and PTH concentrations to document control and prevent adverse effects of toxicosis.
DIAGNOSTIC EVALUATION
Recipient cats
Perform a thorough screening of a potential transplant recipient to identify abnormalities and concurrent diseases before transplant referral. A typical required preoperative diagnostic protocol as well as conditions that preclude transplantation are listed in Table 1 and Table 2, respectively.

Table 2 Conditions That May Preclude Kidney Transplantation in Cats
Obtain a minimum database including a complete blood count, serum chemistry profile, urinalysis, urine culture, and serum total thyroxine concentration. Any cat with a negative urine culture result but with a history of urinary tract infection should undergo a two- to three-week cyclosporine challenge followed by a second urine culture. If a positive culture result is obtained, institute treatment for presumptive chronic pyelonephritis and obtain a second culture after treatment. A second positive culture result eliminates the cat as a potential transplant recipient.
Feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) infections are contraindications to transplantation because of the theoretically increased risk of secondary infections once immunosuppression is initiated.
A serum titer against Toxoplasma gondii antibodies does not signify active infection, but candidates should be considered at higher risk of developing clinical toxoplasmosis after immunosuppression.31 The best course of action to prevent possible recrudescence of infection in antibody-positive recipient cats is unclear; recommendations vary among institutions, with treatment with clindamycin varying from a two-week course before transplantation to lifelong therapy.31,32
Perform blood typing, and identify multiple compatible donors before surgery. Crossmatching typically occurs after patient transfer to the transplant center.
Hyperthyroidism is a common concurrent disease in cats with chronic kidney disease. Affected cats are excluded unless definitive treatment is completed before transplantation because hyperthyroidism treatment can further decrease the glomerular filtration rate and exacerbate chronic kidney disease.33
Perform a complete cardiac evaluation to detect underlying cardiomyopathy. Severe cardiac disease is a relative contraindication because of heightened anesthetic risk and anticipated shortened life span.
Donor cats
The diagnostic evaluation of a donor cat is similar to that described for the recipient. Specific investigation of urinary tract anatomy and function is performed by using abdominal ultrasonography, excretory urography, or computed tomography angiography.34 Cats positive for anti-Toxoplasma gondii antibodies are no longer used as donors. Ethical concerns have arisen regarding the use of living feline donors for kidney transplantation. In people, the risk of mortality associated with kidney donation is about 0.03%.35 Similar nominal risks have been observed in donor cats undergoing unilateral nephrectomy. In one study, no perioperative deaths were reported, and serum creatinine and urea nitrogen concentrations remained within reference ranges.36 Most transplant programs also require adoption of the donor cat, regardless of the outcome of the recipient.
IMMUNOMODULATION
The crucial advance that made clinical organ transplantation feasible between unrelated individuals was the development of immunosuppressive drugs to prevent or control rejection. Foreign tissue rejection is determined by T cell-mediated recognition of cell surface major histocompatibility complex proteins and the peptides they display. Transplanting kidney allografts from unrelated, histoincompatible feline donors results in an acute rejection within five to eight days.37
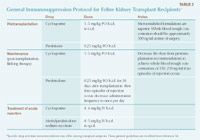
Table 3 General Immunosuppression Protocol for Feline Kidney Transplant Recipients*
Organ transplant recipients are maintained on lifelong immunosuppressive therapy to prevent rejection of the foreign allograft (Table 3). The most current protocols include combination therapy using microemulsified cyclosporine and prednisone.16 Some transplant institutions recommend administering cyclosporine for two weeks before surgery to ensure adequate serum trough levels at the time of surgery, thus preventing initiation of a host vs. graft immune response. Cyclosporine is usually administered at 3 to 5 mg/kg given orally every 12 to 24 hours to obtain whole blood trough concentrations of 500 ng/ml for the first month, then 150 to 250 ng/ml for life.16,38 Immunosuppressive prednisolone therapy is also initiated just before surgery at 0.25 mg/kg given orally every 12 hours, adjusting to once daily after 30 days.16,38
Multiple agents have been known to alter cyclosporine metabolism by increasing the blood cyclosporine concentration and reducing cyclosporine elimination. A regimen using ketoconazole with cyclosporine allows a significant reduction in the cyclosporine dose in people after kidney transplantation.39 The same drug interaction has been demonstrated in cats.40 The benefit is the possibility of once-daily dosing and a lower cost. The disadvantages are the additional pilling requirements and ketoconazole-associated hepatotoxicosis. Comparison studies are still lacking to provide a substantial advantage over the current protocols used.
TRANSPLANT PROCEDURE OVERVIEW
Anesthesia and preoperative management
Anesthesia of patients with end-stage kidney disease is challenging because of altered renal physiology and pharmacokinetics. Chronic kidney disease affects the hematopoietic, cardiovascular, neurologic, metabolic, endocrine, gastrointestinal, pulmonary, and immunologic systems in individual and interrelated ways. Many characteristic metabolic derangements are present in transplant patients including anemia, acidemia, hyperphosphatemia, hypocalcemia, and uremia. Identification of any dysfunction within these body systems should be performed preoperatively so that correction may be attempted if possible.
Preoperative management of the transplant patient includes parenteral fluid diuresis with balanced electrolyte solutions. If treatment with recombinant human erythropoietin and subsequent transplant delay is inappropriate, anemic patients are given blood transfusions to achieve a PCV of > 30% before surgery. Immunosuppressive therapy is continued the day of surgery, as described earlier. Placing a jugular catheter is ideal to monitor hemodynamic parameters before, during, and after surgery.
A standard premedication and anesthetic protocol including an anticholinergic, an opioid, and an inhalant anesthetic agent is used based on the preoperative evaluation and an individual anesthesiologist's preference. Perioperative broad-spectrum antibiotics are administered for the duration of the procedure. Atracurium besylate is used as needed to maintain muscular relaxation during microvascular anastomosis. Dopamine may be administered as a continuous-rate infusion to ensure adequate systolic blood pressure. Mannitol may be given to induce osmotic diuresis in all donor cats before nephrectomy, as well as in recipient cats after vascular anastomosis.38 Administering mannitol may minimize acute tubular necrosis associated with temporary ischemia that occurs during transplantation. A recent report demonstrated that preserving nephrectomized kidneys in cold sodium gluconate or phosphate-buffered sucrose solutions for up to seven hours had no negative impact on patient survival.41
Intraoperatively, standard physiologic parameters are measured continuously, and drug adjustments are made if needed. Arterial or venous blood gas and electrolytes are assessed periodically, and imbalances are corrected as necessary.
Surgery
Donor cats. The donor kidney is removed through a ventral midline celiotomy. Vascular dissection is assisted by using magnifying loupes or a dissecting microscope. Assessment of both donor kidneys is performed, although the left kidney is preferred because of the increased length of the vascular pedicle.42 The donor kidney must be supplied by a single artery (some cats have two arteries supplying a single kidney), and a minimum length of 0.5 cm is generally required to complete the arterial anastomosis.42 The accompanying renal vein is measured to create a sterile template to guide the creation of the donor phlebotomy site. The entire length of the ureter is isolated from the kidney to the urinary bladder before nephrectomy.
Several techniques for vascular anastomosis and ureteral implantation in cats have been described in the literature. Recent reports detail anastomosis of the donor kidney vessels to the postrenal aorta and vena cava.43 Cats in previous studies suffered rear limb complications when the external iliac vessels were used for anastomosis.43
Recipient cats. The surgical approach in the recipient cat is similar to that in the donor cat. The area between the left renal artery and caudal mesenteric artery is isolated and exposed in preparation for the graft. The donor kidney is harvested only after the recipient vessels are prepared for graft implantation. The donor renal artery is anastomosed end-to-side to the aorta by using 8-0 to 10-0 nylon in a simple interrupted pattern.42 The renal vein is anastomosed to the caudal vena cava with two rows of simple continuous sutures with 7-0 silk.43
Several techniques for implanting the ureter into the urinary bladder have been described. Using an extravesicular ureteroneocystostomy is associated with the quickest resolution of renal pelvic dilation after transplantation, and mucosal apposition of the ureter to the bladder significantly reduces the incidence of postoperative obstruction.44,45 To prevent torsion of the transplanted kidney on its pedicle, the renal capsule is attached to the abdominal body wall after creating a peritoneal-transverse abdominis muscle flap.42 One of the recipient's diseased kidneys is biopsied for diagnostic and prognostic purposes, but the native organs are left in place and only removed at a later date if necessary. For postoperative nutritional support, a gastric or esophageal feeding tube is placed before recovery (if not already placed).
Postoperative recovery
Transplant patients are kept free of stress, and handling is minimized. Balanced electrolyte solutions are continued and supplemented as needed to correct acid-base or electrolyte abnormalities. Blood pressure must be monitored frequently during the first 12 to 24 hours, as postoperative hypertension may be severe.46 Supplemental nutrition is provided through gastrostomy or esophagostomy tubes until oral food and water are accepted. PCV, total plasma protein concentrations, serum creatinine concentrations, serum electrolyte concentrations, and trough whole blood cyclosporine concentrations are assessed daily. Voided urine is collected to assess urine specific gravity and determine 24-hour urine output. Renal function and hemodynamic parameters usually return to normal within three to five days after surgery.13 If the transplant recipient remains anorectic or depressed or the serum creatinine concentration continues to rise with production of isosthenuric urine, then graft rejection should be suspected.37 An ultrasonographic examination of the urinary tract should be performed to assess renal graft perfusion, as well as to identify any hydronephrosis or hydroureter. These latter conditions usually suggest stricture at the site of ureter implantation rather than transplant rejection, and surgical intervention may be required rather than changes in medication regimen.
No specific protocol is required for recovery or monitoring of the donor cats in the immediate postoperative period. These patients are managed routinely as with any other post-laparotomy patient (e.g. incision care, analgesia). Transplant institutions will recheck donor patients' serum creatinine concentrations before discharging the cats to their new owners.
Immediate postoperative complications
Immediate postoperative complications including acute graft rejection, hypertension, and neurologic signs have been reported, although immunosuppressive protocols have vastly decreased the incidence of acute rejection episodes.13,46,47 Nineteen presumptive episodes of allograft rejection were noted in 12 of 66 (18%) cats, most commonly in the first two months after surgery.13 Antirejection therapy in cats consists of methylprednisolone sodium succinate, with some transplant centers also giving intravenous cyclosporine to maintain therapeutic serum concentrations.38 Reactivation of chronic feline respiratory viral infections can also be a serious complication.32
Hypertension is a common complication that can occur intraoperatively as well as shortly after surgery. Severe postoperative hypertension requiring intervention (systolic blood pressure > 170 mm Hg) was documented in 62% of recipient cats.46 Managing hypertension has also been shown to significantly reduce the prevalence of neurologic complications.46 Central nervous system disorders have been reported in 21% of cats receiving transplants, with seizures occurring in 88% of these cases.47
LONG-TERM MANAGEMENT AND COMPLICATIONS
Recipient cats. Patients are discharged from the hospital when the graft function appears satisfactory and blood cyclosporine concentrations are stable. Satisfactory graft function is indicated by an adequate nutritional intake and urine concentrating ability, a decreased serum creatinine concentration, and a good attitude.
Successful long-term survival of transplant patients is achieved with good patient and client compliance and continued care by the transplant center, primary care veterinarian, and local emergency clinics. Perform weekly examinations for four weeks. At each visit, determine serum creatinine concentrations, PCV, total solids concentration, body weight, and whole blood cyclosporine concentrations. Subsequently, perform a complete blood count, serum chemistry profile, urinalysis, urine culture, and cyclosporine concentration several times per year. Rechecks should occur frequently (every two to three months minimum) in the first year after surgery, with more frequent rechecks in patients exhibiting any signs of illness; less frequent rechecks (every three to four months) are indicated in future years.
Aside from the complications discussed in the immediate postoperative period, several long-term adverse effects have been documented. Transplant recipients have an increased susceptibility to infection, presumptively because of immunosuppressive therapy.32 Viral, bacterial, parasitic, coccidial, protozoal, and fungal infections can develop and require unusually intensive treatment and supportive care. Urinary tract infections are most common; antimicrobial therapy should be considered with special concern for any potentially nephrotoxic drugs or drugs that may alter the half-life of cyclosporine. Because of their increased susceptibility to infection, transplant recipients should be housed exclusively indoors. Use standard parasite control and vaccination schedules in these cats. However, killed or inactivated and recombinant or subunit vaccines should be administered when possible rather than attenuated or modified-live products.
Toxoplasmosis has been reported as a rare sequela to transplantation and may be due to transplanting a kidney from a healthy but latently infected donor into an uninfected recipient or through reactivation of a latent infection in a recipient because of immunosuppression.31
Transplant recipients are also at an increased risk for developing neoplasia, particularly lymphoproliferative neoplasms.48,49 In one retrospective study, nine of 95 cats (9.5%) developed malignant neoplasia after renal transplantation and immunosuppression, a frequency higher than that expected in cats that do not undergo this procedure.48 Diabetes mellitus is also more common in transplant recipients, which further increases the risk of infection.50
Donor cats. The long-term risks associated with kidney donation in cats appear to be minimal. Donors presumptively have normal renal function at the time of nephrectomy, and loss of 50% of functional nephrons should not result in azotemia or decreased urine concentrating ability. No regular recheck examination schedule is usually recommended, but measuring a serum creatinine concentration and urine specific gravity one to two months after surgery to establish a baseline, followed by yearly rechecks, is likely reasonable.

Table 4 Institutions Performing Feline Renal Transplantation*
SUMMARY
Despite being a costly and medically intensive option, kidney transplantation has proved to be an effective method for treating some cats with chronic kidney disease. The highest chance of success is achieved through careful patient selection and a close working relationship among the client, primary care veterinarian, and surgical and internal medicine specialists. Standardized preoperative screening and postoperative management protocols exist, with some variation, among institutions that offer kidney transplantation (Table 4). The critical first steps to a successful transplantation are contacting an appropriate transplant center and optimizing the candidate's overall health status.
Jason Bleedorn, DVM*
Barrak Pressler, DVM, DACVIM
Department of Veterinary Clinical Sciences
School of Veterinary Medicine
Purdue University
West Lafayette, IN 47904
*Current address: Department of Surgical Sciences School of Veterinary Medicine University of Wisconsin Madison, WI 53706
REFERENCES
1. Gregory CR, Gourley IM, Kochin EJ, et al. Renal transplantation for treatment of end-stage renal failure in cats. J Am Vet Med Assoc 1992;201(2):285-291.
2. Lund EM, Armstrong PJ, Kirk CA, et al. Health status and population characteristics of dogs and cats examined at private veterinary practices in the United States. J Am Vet Med Assoc 1999;214(9):1336-1341.
3. Watson A. Indicators of renal insufficiency in dogs and cats presented at a veterinary teaching hospital. Aust Vet Practit 2001;31:54-58.
4. Lulich J, Osborne C, O'Brien T, et al. Feline renal failure: questions, answers, questions. Compend Contin Educ Small Anim Pract 1992;14:127-153.
5. Carrel A. Transplantation in mass of the kidneys. J Exp Med 1908;10:98-140.
6. Aisenberg AC. An introduction to immunosuppressants. Adv Pharmacol Chemother 1970;8:31-55.
7. Flechner SM. Cyclosporine: a new and promising immunosuppressive agent. Urol Clin North Am 1983;10(2):263-275.
8. Calne RY, White DJ, Thiru S, et al. Cyclosporin A in patients receiving renal allografts from cadaver donors. Lancet 1978;2(8104-8105):1323-1327.
9. U.S. Renal Data System, USRDS 2006 Annual Data Report: Atlas of End-Stage Renal Disease in the United States, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, MD, 2006.
10. Gregory CR, Kyles AE, Bernsteen L, et al. Results of clinical renal transplantation in 15 dogs using triple drug immunosuppressive therapy. Vet Surg 2006;35(2):105-112.
11. Gregory CR, Gourley IM, Haskins SC, et al. Effects of mizoribine on canine renal allograft recipients. Am J Vet Res 1988;49(3):305-311.
12. Mathews KA, Holmberg DL, Miller CW. Kidney transplantation in dogs with naturally occurring end-stage renal disease. J Am Anim Hosp Assoc 2000;36(4):294-301.
13. Mathews KG, Gregory CR. Renal transplants in cats: 66 cases (1987-1996). J Am Vet Med Assoc 1997;211(11):1432-1436.
14. Aronson LR, Kyles AE, Preston A, et al. Renal transplantation in cats with calcium oxalate urolithiasis: 19 cases (1997-2004). J Am Vet Med Assoc 2006;228(5):743-749.
15. Mehl ML, Kyles AE, Pollard R, et al. Comparison of 3 techniques for ureteroneocystostomy in cats. Vet Surg 2005;34(2):114-119.
16. Bernsteen L, Gregory CR, Kyles AE, et al. Renal transplantation in cats. Clin Tech Small Anim Pract 2000;15(1):40-45.
17. Minkus G, Reusch C, Horauf A, et al. Evaluation of renal biopsies in cats and dogs–histopathology in comparison with clinical data. J Small Anim Pract 1994;35:465-472.
18. Ross SJ, Osborne CA, Kirk CA, et al. Clinical evaluation of dietary modification for treatment of spontaneous chronic kidney disease in cats. J Am Vet Med Assoc 2006;229(6):949-957.
19. King JN, Gunn-Moore DA, Tasker S, et al. Tolerability and efficacy of benazepril in cats with chronic kidney disease. J Vet Intern Med 2006;20(5):1054-1064.
20. Syme HM, Markwell PJ, Pfeiffer D, et al. Survival of cats with naturally occurring chronic renal failure is related to severity of proteinuria. J Vet Intern Med 2006;20(3):528-535.
21. Cowgill LD, James KM, Levy JK, et al. Use of recombinant human erythropoietin for management of anemia in dogs and cats with renal failure. J Am Vet Med Assoc 1998;212(4):521-528.
22. Syme HM, Barber PJ, Markwell PJ, et al. Prevalence of systolic hypertension in cats with chronic renal failure at initial evaluation. J Am Vet Med Assoc 2002;220(12):1799-1804.
23. Elliott J, Barber PJ, Syme HM, et al. Feline hypertension: clinical findings and response to antihypertensive treatment in 30 cases. J Small Anim Pract 2001;42(3):122-129.
24. Jepson RE, Elliott J, Brodbelt D, et al. Effect of control of systolic blood pressure on survival in cats with systemic hypertension. J Vet Intern Med 2007;21(3):402-409.
25. Mathur S, Syme H, Brown CA, et al. Effects of the calcium channel antagonist amlodipine in cats with surgically induced hypertensive renal insufficiency. Am J Vet Res 2002;63(6):833-839.
26. Goldstein RE, Marks SL, Kass PH, et al. Gastrin concentrations in plasma of cats with chronic renal failure. J Am Vet Med Assoc 1998;213(6):826-828.
27. Kraut JA, Kurtz I. Metabolic acidosis of CKD: diagnosis, clinical characteristics, and treatment. Am J Kidney Dis 2005;45(6):978-993.
28. Dow SW, Fettman MJ, Curtis CR, et al. Hypokalemia in cats: 186 cases (1984-1987). J Am Vet Med Assoc 1989;194(11):1604-1608.
29. Cheng S, Coyne D. Vitamin D and outcomes in chronic kidney disease. Curr Opin Nephrol Hypertens 2007;16(2):77-82.
30. Polzin DJ, Ross SJ, Osborne CA, et al. Clinical benefit of calcitriol in canine chronic kidney disease [abst]. J Vet Intern Med 2005;19:433.
31. Bernsteen L, Gregory CR, Aronson LR, et al. Acute toxoplasmosis following renal transplantation in three cats and a dog. J Am Vet Med Assoc 1999;215(8):1123-1126.
32. Kadar E, Sykes JE, Kass PH, et al. Evaluation of the prevalence of infections in cats after renal transplantation: 169 cases (1987-2003). J Am Vet Med Assoc 2005;227(6):948-953.
33. Graves TK, Olivier NB, Nachreiner RF, et al. Changes in renal function associated with treatment of hyperthyroidism in cats. Am J Vet Res 1994;55(12):1745-1749.
34. Bouma JL, Aronson LR, Keith DG, et al. Use of computed tomography renal angiography for screening feline renal transplant donors. Vet Radiol Ultrasound 2003;44(6):636-641.
35. Matas AJ, Bartlett ST, Leichtman AB, et al. Morbidity and mortality after living kidney donation, 1999-2001: survey of United States transplant centers. Am J Transplant 2003;3(7):830-834.
36. Lirtzman RA, Gregory CR. Long-term renal and hematologic effects of uninephrectomy in healthy feline kidney donors. J Am Vet Med Assoc 1995;207(8):1044-1047.
37. Kyles AE, Gregory CR, Griffey SM, et al. Evaluation of the clinical and histologic features of renal allograft rejection in cats. Vet Surg 2002;31(1):49-56.
38. Katayama M, McAnulty JF. Renal transplantation in cats: techniques, complications, and immunosuppression. Compend Contin Educ Small Anim Pract 2002;24:874-882.
39. el-Agroudy AE, Sobh MA, Hamdy AF, et al. A prospective, randomized study of coadministration of ketoconazole and cyclosporine A in kidney transplant recipients: ten-year follow-up. Transplantation 2004;77(9):1371-1376.
40. McAnulty JF, Lensmeyer GL. The effects of ketoconazole on the pharmacokinetics of cyclosporine A in cats. Vet Surg 1999;28(6):448-455.
41. McAnulty JF. Hypothermic storage of feline kidneys for transplantation: successful ex vivo storage up to 7 hours. Vet Surg 1998;27(4):312-320.
42. Gregory C. Renal transplantation in cats. Compend Contin Educ Small Anim Pract 1993;15:1325-1338.
43. Bernsteen L, Gregory CR, Pollard RE, et al. Comparison of two surgical techniques for renal transplantation in cats. Vet Surg 1999;28(6):417-420.
44. Kochin EJ, Gregory CR, Wisner E, et al. Evaluation of a method of ureteroneocystostomy in cats. J Am Vet Med Assoc 1993;202(2):257-260.
45. Gregory CR, Lirtzman RA, Kochin EJ, et al. A mucosal apposition technique for ureteroneocystostomy after renal transplantation in cats. Vet Surg 1996;25(1):13-17.
46. Kyles AE, Gregory CR, Wooldridge JD, et al. Management of hypertension controls postoperative neurologic disorders after renal transplantation in cats. Vet Surg 1999;28(6):436-441.
47. Gregory CR, Mathews KG, Aronson LR, et al. Central nervous system disorders after renal transplantation in cats. Vet Surg 1997;26(5):386-392.
48. Wooldridge JD, Gregory CR, Mathews KG, et al. The prevalence of malignant neoplasia in feline renal-transplant recipients. Vet Surg 2002;31(1):94-97.
49. Gregory CR, Madewell BR, Griffey SM, et al. Feline leukemia virus-associated lymphosarcoma following renal transplantation in a cat. Transplantation 1991;52(6):1097-1099.
50. Case JB, Kyles AE, Nelson RW, et al. Incidence of and risk factors for diabetes mellitus in cats that have undergone renal transplantation: 187 cases (1986-2005). J Am Vet Med Assoc 2007;230(6):880-884.