Skills Laboratory: How to perform a positive contrast gastrointestinal study
Add a little contrast to help you find your diagnosis.
Step 1 >
Positive contrast gastrointestinal (GI) studies are performed to help diagnose suspected GI disease after a negative or questionable preliminary radiographic examination. GI contrast studies can be difficult to interpret, so to increase the probability of an accurate diagnosis, it is important to perform the procedure correctly, with a properly prepared patient, the correct amount of contrast agent, and the correct positioning, radiographic technique, and radiographic views. A positive contrast GI study should be performed in patients in which radiographs, additional imaging, and the clinical assessment do not yield a sufficient diagnosis.
Many positive contrast GI studies have been replaced with ultrasonography and endoscopy when these tools are available. While ultrasonography is useful in many GI studies, it is very user-dependent and can be challenging for individuals who are not thoroughly trained, making a positive contrast GI study more practical in many situations.
INDICATIONS AND CONTRAINDICATIONS
A positive contrast GI study is commonly used to evaluate GI transit time, GI motility, the mucosal surface, GI content, GI strictures, and GI obstruction including foreign bodies and masses.
Specific indications include:
- Acute and continual or recurrent vomiting (including hematemesis) without related findings on survey radiographs
- A suspected GI obstruction or history of foreign body ingestion
- A palpable abdominal mass without an obstructive GI pattern on survey films
- An unexplained organ displacement
- An abnormal appearance of the stomach or small intestines on survey radiographs
- Weight loss with associated diarrhea
- Melena
- Acute abdominal pain with questionable abnormalities seen on survey radiographs.
Contraindications include:
- Intractable vomiting, because it causes an increased risk of aspiration
- Suspected perforation with or without evidence of free peritoneal gas or loss of serosal detail (use nonionic iodinated contrast medium)
- An evident need for surgery on the survey radiographs
- A fractious and unmanageable patient, making administration of the contrast agent impossible without heavy sedation or anesthesia.
Why do contrast radiography?
Performing a positive contrast GI study is an important diagnostic procedure, especially when advanced imaging such as ultrasonography is not available or there are financial limitations. When performed correctly, a positive contrast GI study can provide supportive diagnostic information that may be useful to a client in making a decision on whether or not to proceed with an invasive or expensive procedure. These studies are minimally invasive and have minimal risk when performed correctly. But be sure to explain to clients the benefits and limitations of a positive contrast GI study.
Keep in mind that the results can be difficult to interpret. To increase the probability of a correct diagnosis, you must perform a complete study. If the study is incomplete, multiple artifacts can be created, decreasing the probability of an accurate diagnosis by increasing the probability of false negative and false positive results.
Step 1: Initially prepare the patient
For an elective positive contrast GI study, patients should be fasted for 12 to 24 hours, and water should be withheld for at least two hours before the contrast study. The ideal prepared patient has a completely empty stomach so that a true transit time can be evaluated. Some emergency situations or time-sensitive clinical signs do not allow for patient preparation.
Step 2: Take survey images
Obtain survey radiographs to make a tentative diagnosis and determine whether a contrast study is necessary, determine whether the patient is properly prepared, and make the necessary corrections to the radiographic technique to optimize a diagnosis.
Properly position the patient for an upper GI study. Obtain survey radiographs of the abdomen with at least two orthogonal views that include the entire abdomen from the diaphragm to the femoral heads (Figures 1A & 1B).

Figure 1A

Figure 1B
If gastric content is present and it is not an emergency, delay the study. A warm water enema may be necessary if there is fecal content within the colon obscuring visualization of the stomach; the patient should be re-evaluated at least one hour later if time permits. If a pyloric abnormality is suspected, obtain a left lateral image for evaluation.
Step 3: Prepare the patient for contrast agent administration
To prepare the patient, sedation is not desirable and should be avoided because there are few drugs that do not have a side effect on GI transit time. If sedation is a necessity, certain drugs and doses are recommended that have minimal effects on the GI system.
- Dogs-Acepromazine: 0.025 to 0.2 mg/kg intravenously (maximum 3 mg) or 0.1 to 0.25 mg/kg intramuscularly1
- Cats-Ketamine: 5 mg/kg and diazepam: 0.2 mg/kg intravenously1; or ketamine: 2.7 mg/kg and diazepam: 0.09 mg/kg intramuscularly in separate syringes.2
Next, decide whether to use barium or an iodinated contrast agent (e.g. iohexol).
Use an iodinated contrast agent when perforation is suspected. Barium leakage within the peritoneal cavity can cause foreign body granulomas, peritonitis, and adhesions. Iodinated contrast agents are satisfactory to look for obstruction, but they do not adhere to the mucosal surface, so they are poor contrast agents to evaluate the GI surface.
There are two types of iodinated contrast agents-nonionic and ionic. Nonionic iodinated contrast agents such as iohexol are safer than ionic iodinated contrast agents such as iothalamate because ionic iodinated contrast agents are more hypertonic, which can cause an influx of fluid into the GI tract that dilutes the contrast agent and can cause electrolyte imbalances and worsen dehydration.
Calculate the dose of the contrast agent, and pull it up into an appropriate syringe for oral administration (Table 1). It is important to give the patient the complete dose of the contrast agent, so oral administration by an orogastric tube is recommended.
Table 1: Correct Dosage of Contrast Agents for Dogs and Cats
DOGS
Micropulverized barium solution 30% to 60% weight/volume
- <20 kg: 8 to 12 ml/kg
- >20 kg: 5 to 7 ml/kg
Iodinated contrast agent: Iohexol diluted
- Dehydration should be corrected before administration
- 700 to 875 mg of iodine/kg diluted with water to obtain a whole volume of 10 ml/kg
CATS
Micropulverized barium solution 30% to 60% weight/volume
- 12 to 20 ml/kg
Iodinated contrast agent: Iohexol diluted
- Dehydration should be corrected before administration
- 600 to 800 mg of iodine/kg diluted with water to obtain a whole volume of 10 ml/kg
Step 3 cont'd
Figure 2A shows the supplies needed for administration of contrast agents by stomach tube. Contrast can be given orally by syringe, but it increases the likelihood of leakage out of the mouth and an incomplete dose of contrast agent being given. An incomplete dose affects transit time and complete distention of the intestinal structures.

Figure 2A
Step 3 cont'd
An incomplete dose of contrast media is the most frequent cause of a nondiagnostic positive contrast GI study. Figure 2B is an example of a radiograph with a complete dose of contrast agent that distends the stomach and intestinal structures.
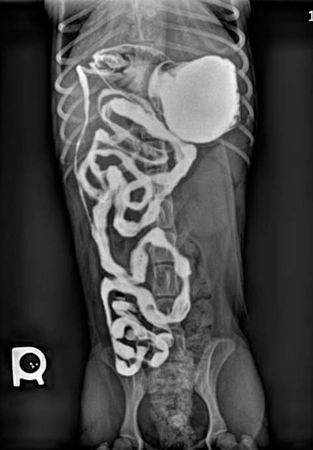
Figure 2B
Figure 2C is an example of a radiograph showing minimal contrast agent in the stomach and intestines, making it unclear whether the filling defect is the result of lack of distention (incomplete dose) or pathology.

Figure 2C
Step 4: Place an orogastric tube
Use a well-lubricated tube. Measure from the end of the patient's nose to the last rib with the tube, and mark the tube appropriately with a marker or tape (Figure 3A). Measuring the tube will help avoid passage of the tube too far, which can lead to damage or perforation of a diseased gastric wall.

Figure 3A
Step 4 cont'd
After the tube is measured, place a mouth gag in the patient's mouth that is safe in an animal that is awake. A commonly used economical mouth gag is a 0.5-in or 1-in roll of tape (Figure 3B). For cats you may use a 0.5-in roll of tape (with some of the tape previously used so the roll is smaller) and smaller orogastric tubing.

Figure 3B
Step 4 cont'd
Advance the orogastric tube into the mouth and down the esophagus to the measured and marked area on the tubing (Figure 3C). Once the tubing is passed, the patient is ready for contrast agent administration. Depending on the size of the tubing, a regular tipped syringe with or without a Christmas tree adapter or a catheter-tipped syringe can be used.

Figure 3C
If you want to be sure the tube has passed into the esophagus, you can palpate the neck and feel for two discrete tubes (the trachea and the orogastric tube), obtain a radiograph, or pass a small amount water into the tube to ensure the patient does not cough, which would be suggestive of the fluid entering the bronchial tree. The probability of your passing an orogastric tube into the trachea when it is the proper length and there is no resistance is very low.
Step 5: Administer the contrast agent, and take the radiographic images
Administer the contrast agent. Add a small amount of air or water into the orogastric tube after administration to ensure that the entire dose is received and no contrast agent is left within the tubing. Figures 4A & 4B were obtained immediately after contrast agent administration.

Figure 4A

Figure 4B
Step 5 cont'd
Table 2 lists the sequence of images to be obtained. Be sure to mark all images with a time and R/L marker.
Table 2: Sequence of Image Acquisition in Dogs and Cats
DOGS
Barium administration*
- Immediate right lateral, left lateral, ventrodorsal, and dorsoventral images
- Right lateral and ventrodorsal images every 30 minutes until the contrast agent reaches the colon and completely leaves the stomach or an obstruction is identified
Iodinated contrast agent administration
- Immediate right lateral, left lateral, ventrodorsal, and dorsoventral images
- Right lateral and ventrodorsal images at 15, 30, 60, 90, 120, and 150 minutes and every 20 minutes until the contrast reaches the colon and leaves the stomach or an obstruction is identified
CATS
Barium administration*
- Immediate right lateral, left lateral, ventrodorsal, and dorsoventral images
- Right lateral and ventrodorsal images at 15, 30, 60 minutes and every 30 minutes until the contrast reaches the colon and completely leaves the stomach or an obstruction is identified
Iodinated contrast agent administration
- Immediate right lateral, left lateral, ventrodorsal, and dorsoventral images
- Right lateral and ventrodorsal images at 15, 30, 45, 60, 75, and 90 minutes and every 15 minutes until the contrast agent reaches the colon and leaves the stomach or an obstruction is identified
*Source: Wallack ST. Handbook of veterinary contrast radiography. San Diego, Calif: San Diego Veterinary Imaging, 2003.
Step 6: Make a diagnosis
Figures 5A-5F are from a normal upper GI study in a dog, which you can use as a comparison for your patients.
Figures 5A & 5B: Thirty minutes after administration, the contrast agent has traveled through most of the small intestines, and a portion of the contrast agent still remains in the stomach.
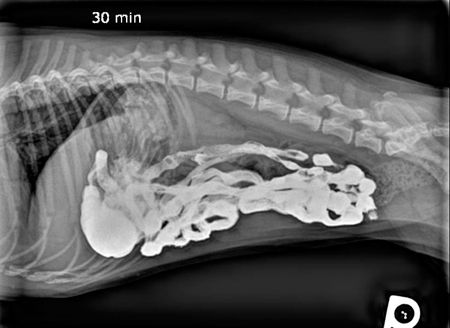
Figure 5A

Figure 5B
Step 6 cont'd
Figures 5C and 5D: One hour after administration, less contrast agent is in the stomach. The contrast agent has still not reached the large intestines, and most of the contrast agent remains in the small intestines, showing normal GI passage of the contrast agent and a normal transit time.

Figure 5C

Figure 5D
Step 6 cont'd
Figures 5E and 5F: Two and a half hours after administration, the contrast agent has reached the colon, and the stomach is empty (normal transit time).

Figure 5E

]
Figure 5F
< Back
Tips to help make an accurate diagnosis
- Evaluate the size, shape, and location of the GI structures.
- Evaluate transit times and use references for normal times (see Suggested Reading).
- Evaluate intestinal patency.
- Look for repeatable focal narrowing of the lumen or contrast agent column.
- Look for a space-occupying lesion.
- Evaluate whether the rugal folds or the mucosal surfaces are abnormal.
- Evaluate whether a smooth interface between the contrast and mucosal surface is present.
- Evaluate the wall of the bowel.
- Determine whether the pylorus opens to permit expulsion of the contrast.
- Note if you document a suspicious finding on multiple radiographs over time.
- When in doubt, send it out. If you are unfamiliar with interpreting GI studies or unsure about the results, send the images to a radiologist or a radiology reading service.
REFERENCES
1. Wallack ST. Handbook of veterinary contrast radiography. San Diego, Calif: San Diego Veterinary Imaging, 2003.
2. Thrall DE. The small bowel. In: Textbook of veterinary diagnostic radiology. 5th ed. Philadelphia, Pa: Saunders Elsevier, 2007;771-775.
SUGGESTED READING
1. Miyabayashi T, Morgan JP, Atitola MAO, et al. Small intestinal emptying time in normal beagle dogs. Vet Radiol 1986;27:164-168.
2. Gomez JA. The gastrointestinal contrast study-methods and preparation. Vet Clin North Am 1974;4(4):805-842.
3. Morgan JP. The upper gastrointestinal tract in the cat: a protocol for contrast radiography. Vet Radiol 1977;18(5):134-137.
4. Agut A, Sanchez-Valverde MA, Lasaosa JM, et al. Use of iohexol as a gastrointestinal contrast medium in the dog. Vet Radiol 1993;34(3):171-177.
5. Williams J, Biller DS, Miyabayashi T, et al. Evaluation of iohexol as a gastrointestinal contrast medium in normal cats. Vet Radiol 1993;34(5):310-314.