Toxicology Brief: Baclofen overdose in dogs
Baclofen is a centrally acting skeletal muscle relaxant.
Baclofen (Lioresal—Novartis) is a centrally acting skeletal muscle relaxant. It is used to control spasticity and pain in people with multiple sclerosis and spinal disorders. Baclofen has also been used extralabel in dogs (1 to 2 mg/kg orally t.i.d.) to treat urinary retention by reducing urethral resistance.1 It is available in 10- and 20-mg tablets and as a parenteral injection.
Mechanism of action and pharmacokinetics
Baclofen mimics γ-aminobutyric acid (GABA) within the spinal cord and works by depressing monosynaptic and polysynaptic afferent reflex activity at the spinal cord level, thereby reducing skeletal muscle spasm caused by upper motor neuron lesions.2 The overall effect is a flaccid paralysis of skeletal muscles. When administered intrathecally, baclofen also inhibits substance P, a stimulatory compound within the brainstem, and it reduces myocardial epinephrine and norepinephrine content.2,3 At oral therapeutic concentrations, baclofen has virtually no central nervous system effects because of its poor ability to cross the blood-brain barrier, but in overdose situations, central nervous system effects are common.4
Baclofen is rapidly and completely absorbed from the gastrointestinal tract and reaches peak blood concentrations in two or three hours in people; however, in an overdose situation, absorption may be prolonged over several hours.2,5 The onset of clinical signs after acute oral exposure may be rapid (within 30 to 60 minutes) or may be delayed for several hours.2 In a survey of 40 dogs with baclofen toxicosis, the onset of signs occurred as early as 15 minutes after exposure and as late as seven hours after exposure (average of 1.9 hr) (ASPCA Animal Poison Control Center [APCC] Database: Unpublished data, 1994-2004).
The half-life of baclofen in people is two and a half to four hours, but in overdose situations the half-life has been reported to increase to as much as 34 hours because of saturation of metabolic and elimination mechanisms.5 The duration of clinical signs in animals with baclofen intoxication has varied from several hours to several days.4 Signs can continue long after serum baclofen concentrations have returned to normal because of the slow clearance from the central nervous system (ASPCA APCC Database: Unpublished data, 1994-2004). Baclofen has low protein-binding (30%) and a wide volume of distribution. About 80% of the drug is eliminated unchanged in the urine, with 15% to 20% undergoing hepatic metabolism and biliary excretion.4,6 Baclofen is principally metabolized by deamination in the liver, but there is also some deamination in the renal tubules.6
Clinical signs and toxicity
Most cases of baclofen toxicosis reported to the ASPCA APCC have involved dogs ingesting their owners' medication (ASPCA APCC Database: Unpublished data, 1994-2004). The most common clinical signs of toxicosis are vomiting, ataxia, and vocalization or disorientation, but the most life-threatening signs are dyspnea, respiratory arrest, and seizures. Dyspnea and respiratory arrest are secondary to paralysis of the diaphragm and intercostal muscles. The mechanism for baclofen-induced seizures is thought to be decreased GABA release from presynaptic neurons, resulting in excessive postsynaptic firing.4 Other frequent clinical signs of baclofen toxicosis include salivation, depression, coma, weakness, recumbency, and hypothermia. Hypotension, bradycardia, hyperactivity or agitation, tremors, panting, mydriasis, diarrhea, respiratory arrest, pulmonary edema, and death have been reported less frequently (ASPCA APCC Database: Unpublished data, 1994-2004) (Table 1).
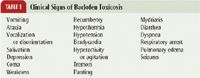
Table 1: Clinical Signs of Baclofen Toxicosis
The oral LD50 in rats and mice is high (145 and 200 mg/kg, respectively),6 but dogs appear to be more sensitive. Doses as low as 1.3 mg/kg caused vomiting, depression, and vocalizing in a 3-month-old rottweiler (ASPCA APCC Database: Unpublished data, 1994-2004). There are no established lethal doses in dogs, but per the ASPCA APCC database, deaths in dogs have occurred at doses estimated to be between 8 and 16 mg/kg.
Treatment
Because of the potential for a rapid onset of clinical signs, decontamination is best attempted under veterinary supervision. Emesis is contraindicated in symptomatic animals. Activated charcoal with a cathartic is recommended; however, repeated doses of activated charcoal have not been proved to be beneficial. Avoid magnesium-based cathartics, as they may compound central nervous system depression.4 Gastric lavage may be considered in cases of large ingestions, but take care to ensure that anesthesia does not compound central nervous system depression. Using short-acting induction agents such as propofol or thiopental sodium followed by inhalant anesthesia is preferred, and the airway must be protected.
Because of baclofen's low protein-binding and urinary excretion, its elimination may be enhanced through fluid diuresis.4 Fluid therapy will also help maintain blood pressure, protect the kidneys from myoglobinuria (secondary to tremors or seizures), and may aid in reducing cardiac arrhythmias.4 Cardiac monitoring with electrocardiography is recommended, and refractory arrhythmias should be treated as needed. Hypothermia is common in comatose or recumbent patients, so thermoregulation is important.
Ventilatory support is a prime concern, and endotracheal intubation and positive pressure mechanical ventilatory support may be needed for an extended time in severe cases. Monitor for aspiration in comatose animals. The use of central nervous system respiratory stimulants is of questionable value.4 Flumazenil and physostigmine have been used in people with baclofen toxicosis, with varying results.6 Experimental studies of baclofen toxicosis in rats have failed to consistently produce positive outcomes when flumazenil was used, and the drug can cause serious adverse effects (seizures).6 Phaclofen is a baclofen reversal agent that has been used experimentally, but it is not commercially available.6
Diazepam (0.5 to 1 mg/kg slowly intravenously, to effect) is the drug of choice for baclofen-induced seizures.4 Propofol or isoflurane may be considered in cases that are refractory to diazepam. Take care when administering long-acting barbiturates or other agents that produce profound or prolonged central nervous system depression in animals experiencing seizures. Cyproheptadine hydrochloride (1.1 mg/kg orally or rectally, as needed) has been used with some success to reduce the vocalization or disorientation seen in some animals (ASPCA APCC Database: Unpublished data, 1994-2004).
Hypoglycemia, hypokalemia, and elevated serum creatine phosphokinase, L-lactate dehydrogenase, and aspartate transaminase activities have occasionally been reported in people with baclofen toxicosis, so obtain baseline serum chemistry profile, acid-base balance, and electrolyte values.6 Continue to monitor these values and correct any abnormalities until signs have resolved. Baclofen concentrations can be determined in urine and serum, although they are considered of minimal benefit in managing clinical cases of toxicosis.4
Prognosis
Resolution of clinical signs may take several days in severe cases, but if adequate ventilatory support is available, the prognosis is generally good. Animals experiencing seizures have a more guarded prognosis. After a patient has recovered from baclofen toxicosis, no residual central nervous system effects are expected. No specific gross or histopathologic lesions would be expected in animals that die of skeletal muscle relaxant toxicosis.
"Toxicology Brief" was contributed by Tina Wismer, DVM, DABVT, DABT, ASPCA Animal Poison Control Center, 1717 S. Philo Road, Suite 36, Urbana, IL 61802. The department editor is Petra A. Volmer, DVM, MS, DABVT, DABT, College of Veterinary Medicine, University of Illinois, Urbana, IL 61802.
REFERENCES
1. Lane, I.: Urinary obstruction and functional urine retention. Textbook of Veterinary Internal Medicine: Diseases of the Dog and Cat (S.J. Ettinger; E.C. Feldman, eds.). W.B. Saunders, Philadelphia, Pa., 2000; pp 93-96.
2. Baclofen. AHFS Drug Information. American Society of Health-System Pharmacists, Inc., Bethesda, Md., 2000; pp 1265-1269.
3. Ellenhorn, M.J.: Muscle relaxants. Ellenhorn's Medical Toxicology: Diagnosis and Treatment of Human Poisoning, 2nd Ed. Lippincott, Williams & Wilkins, Baltimore, Md., 1997; pp 937-953.
4. Shannon, M.W.: Muscle relaxants. Clinical Management of Poisoning and Overdose, 3rd Ed. (L.M. Haddad et al., eds.). W.B. Saunders, Philadelphia, Pa., 1998; pp 1181-1186.
5. Hecht, D.V.; Allenspach, K.: Presumptive baclofen intoxication in a dog. J. Vet. Emerg. Crit. Care 8:49-54; 1998.
6. POISINDEX editorial staff: Baclofen. POISINDEX System, Vol. 100 (B.H. Rumack et al., eds.). MICROMEDEX, Englewood, Colo., expires 12/00.