Understanding viral zoonoses: H1N1 influenza
Influenza is a zoonotic infection that holds especially high interest of late, although it has been a subject of great fascination for microbiologists for a long time.
Influenza is a zoonotic infection that holds especially high interest of late, although it has been a subject of great fascination for microbiologists for a long time. With the current H1N1 pandemic, it is important that all healthcare workers—including veterinarians—understand how the virus works, why it works so successfully, and what we are doing to treat and stop the spread of this virus.
INFLUENZA BASICS: STRUCTURE AND VIRULENCE FACTORS
Influenza is an RNA virus with eight separate gene sequences, and it holds its genome together like eukaryotic cells with multiple chromosomes. This structure allows hybrids to form between different influenza strains. Furthermore, the virus has a high mutation rate because of inefficient RNA polymerase editing functions, and that allows additional viral variation.
Three matrix forms of influenza exist—A, B, and C. Influenza A and B cause disease in people. Influenza's primary modus operandi is to create epidemic disease among susceptible people, and most of the mortality results from pulmonary complications. The two major antigenic constituents of influenza are hemagglutinin (H) and neuraminidase (N).
Influenza viruses have five basic virulence factors:
1. The F2 sequence of its polymerase targets the virus to the inner and outer mitochondrial membranes, which injures cells by dissipating energy production and inducing intrinsic apoptosis and cell death.
2. A nonstructural protein, NS1, has several characteristics, but the most important is that it inhibits alpha-interferon, which is critical in the host's initial control of influenza. NS1 essentially shuts down a host defense against influenza that results in extensive disease.
3. Hemagglutinin must initially undergo partial proteolysis by host-derived enzymes to allow it to bind to its receptor, so the degree of hemagglutinin's protease susceptibility is a viral virulence factor.
4. Hemagglutinin binds to neuraminic acid, which is the substrate for neuraminidase. The hemagglutinin-neuraminidase ratio has to be just in the right concentration to allow the virus to rapidly invade other cells and to escape from one infected cell to another, and that ratio is important.
5. The lack of immune recognition of the two major epitopes that the virus expresses is a key event, and the reason new H1N1 is so successful—its major antigenic constituents are not previously recognized by the human immune system. So virtually every person is susceptible to a greater or lesser degree to this new strain of influenza.
MAJOR INFLUENZA OUTBREAKS: 1918-2009
In the past century, the most famous influenza outbreak was the Spanish Flu—H1N1—of 1918. That was the only time in recorded history that the world population actually diminished for a short period of time. Then in the 1950s the first episode of the Asian flu, H2N2, occurred. In 1968, the Hong Kong flu, H3N2, occurred, and in 2009, we had swine flu, or new H1N1. The last major pandemic flu occurred more than 40 years ago, and nearly everyone expected that the next pandemic flu would be H5N1—avian flu.
H5N1 is a particularly virulent virus and is of great concern. When this virus leaps from avian species to people, it is a serious disease. More than 100 cases of avian influenza have occurred in people, and the fatality rate is between 40% and 70%—it is 70% in infected people who do not receive antiviral drugs. The Ebola virus has about the same level of lethality associated with it. The good news is that so far H5N1 is inefficiently transmitted from person to person. Only individuals who have had extensive interaction with avian species have contracted this disease.
So rather than avian flu, the next pandemic flu strain evolved right under our noses in Mexico—new H1N1.
Influenza cases were first recognized in March 2009 in Mexico, and by April, the first cases were identified in southern California. Within two months the World Health Organization (WHO) raised its worldwide pandemic alert level to phase 6, which correlates with an uncontrolled pandemic. New H1N1 caused an unprecedented springtime outbreak (in contrast to usual annual influenza-like illness outbreak patterns) and presaged a large epidemic in the usual winter season, which we are in now. As of November 2009, the pandemic alert level was still phase 6, and about 4,000 deaths had been attributed directly or indirectly to new H1N1 in the United States. The median age of infected people who have died is 36 years.
A large number of international travelers who passed through Mexico City in April and May 2009 when the virus was just starting to spread. By the time the WHO realized what was occurring, the virus had become widely distributed. Travelers had already returned to their countries of origin, and the virus had been distributed to several North American and European cities and other parts of the globe. There was no way to control it other than to attempt to deal with its consequences. Keep in mind that based on airline statistics, about 1,000,000 international travelers move from one country to another every week. So controlling influenza spread is difficult.
INFLUENZA RESERVOIRS AND REASSORTMENT
The reservoir for influenza is wild, migratory waterfowl. They carry influenza virus in their gastrointestinal tracts and serve as a natural reservoir for periodic outbreaks in people. New H1N1 is a quadruple reassorted virus that has gene sequences derived from Eurasian swine, classic swine, people, and birds. And even though it is H1N1 and our immune system recognizes its two major antigenic constituents—hemagglutinin and neuraminidase—antibodies to the recently circulating seasonal H1N1 virus offer no or little protection. A substantial variation and mutational rate in the H1 portion has occurred—up to 20 amino acids are different.
THE ROLE OF PIGS IN THE EPIDEMIOLOGY AND SPREAD OF INFLUENZA
Pigs are a good intermediate host to condition influenza viruses to exist in people. Influenza virus is indigenous to waterfowl, and waterfowl interact with domesticated fowl and transmit the virus. Bird-adapted influenza has specific conformational epitopes to bind to host membranes, and the virus particularly likes alpha 2,3-linked sialic acid receptors to bind hemagglutinin. This preference is bad for birds, but people have few alpha 2,3 sialic acid receptors in their respiratory epithelium. The human upper airways (nose, trachea, major bronchi) contain alpha 2,6 sialic acid receptors for hemagglutinin, so people are relatively immune to bird influenza. Unfortunately, pigs express both alpha 2,3 and alpha 2,6 sialic acid receptors in their respiratory and gastrointestinal tracts, so pigs are an intermediate host in which bird-adapted and human-adapted viruses can coexist. The intermixing of these viruses often occurs in pigs, and epidemics often arise, which appears to be the case with the current H1N1 epidemic.
People do have alpha 2, 3 sialic acid-galactose linkages in their lower respiratory apparatus. So if an avian influenza virus passes through the upper airways, it has ample opportunity to cause severe disease in people.
The good news for people is that new H1N1 has low virulence potential. It does not appear to be any more virulent than the typical seasonal influenza that we have been exposed to for the last several decades. It can injure a subset of the population and cause death, but it lacks many of the virulence factors mentioned above. The bad news is that H1N1 is highly transmissible and is approaching transmission rates similar to that of wild-type seasonal influenza, and people have no preexisting immunity, so all are susceptible.
What keeps virologists up at night is the possibility of a viral reassortment leading to an H5N1-H1N1 hybrid that is highly virulent and highly transmissible. If a virus with a 70% mortality rate infects 30% of the world's population in a year, a population die-off would occur.
WHY WAS THE 1918 VIRUS SO VIRULENT?
Probably the most intriguing and disturbing part about the Spanish Flu H1N1 was its hemagglutinin. Virologists recently isolated the virus from victims of the 1918 influenza who had been frozen in the Alaskan tundra. The virologists made hybrids of this virus in order to study it—they took the hemagglutinin of the 1918 Spanish flu and joined it with a mouse-adapted influenza strain. They found that the hemagglutinin of the 1918 virus was adapted to recognize both alpha 2,3 and alpha 2,6 sialic acid linkages. So the virus was able to spread rapidly using its alpha 2,6 binding capabilities in the upper airways, and when it got into the lower airways, where people have alpha 2,3 receptors, it was able to replicate rapidly in lung tissue and cause severe hemorrhagic lung disease.
Fortunately, the new H1N1 virus does not have this capacity and is primarily restricted to alpha 2,6 linkages, although it will cause lower airway disease in some infected people.
In 1918, there were no ventilators, essentially no antibiotics, and no antivirals. So presumably we could do a better job of managing severe influenza today than in 1918. However, some parts of the world still have no ventilators, antibiotics, or antivirals, and a virulent influenza strain could be a severe problem in those places.
WHAT HAPPENS WHEN PEOPLE GET THE FLU?
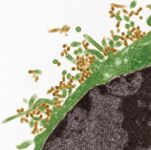
Influenza is not a subtle virus. It enters the host and tries to replicate extensively before an immune response develops. It is then coughed up and transmitted to someone else. The normal human trachea has a sea of cilia that beat continuously throughout our respiratory epithelium, beating at 12 beats/second, 24 hours a day, seven days a week. This system constantly mechanically cleans our airways. But 48 hours after inoculation with nonfatal H3N2 virus, the respiratory epithelium is wiped out, and only goblet cells remain, which are the cells that produce mucus carried by the cilia. Thus, people with influenza readily get secondary bacterial pneumonias.
In fatal cases of new H1N1, typical histologic lesions of primary influenza pneumonia are seen—the alveoli are filled, and type I and type II pneumocyte apoptosis occurs, along with squamous metaplasia of the bronchial epithelium. Hemorrhage occurs throughout the lung tissue, and the respiratory apparatus cannot function. This occurs in only a minority of people who have H1N1 infection—the mortality rate estimate is between 0.1% and 0.01%. So it's a relatively avirulent virus, but it can be severe in certain individuals.
CAN PHYSICIANS RECOGNIZE INFLUENZA JUST BY TALKING TO THEIR PATIENTS?
In the middle of an epidemic, simply talking to people about their symptoms can be diagnostic. Influenza is dissimilar from an upper respiratory infection. Rhinoviruses typically cause a runny nose and a minor sore throat without a fever. Influenza usually has an abrupt onset and is associated with a fever that is often high. Infected people may have a dry cough, a subjective sense of shortness of breath, and severe myalgia, weakness, and general malaise. Some infected individuals also have gastrointestinal symptoms; the upper respiratory viruses do not usually cause diarrhea. Enteric viruses typically cause diarrhea, but influenza viruses can also cause diarrhea, and with H1N1, physicians are seeing a lot of gastrointestinal signs in patients.
Another strikingly different characteristic of pandemic influenza compared with normal seasonal epidemic influenza is the age distribution of the affected population. H1N1 primarily affects young, healthy individuals. People who were born before 1957 while the Spanish Flu virus was still circulating probably have already had experience with this virus and may have acquired some T-cell and even some B-cell immunity related to that exposure. So the older population is perhaps relatively spared from the ravages of this outbreak of H1N1. However, it has been difficult to get the message out to parents and college students about new H1N1 because most people think influenza is something for their grandparents to worry about. But being young and healthy with a good immune system will not protect individuals against H1N1, which is why the vaccine strategy has focused on young people. It does not mean that if you are older you should not get the vaccine when it becomes available. But individuals who are most likely to get H1N1 and develop severe sequelae should receive the vaccine first.
COMPLICATIONS OF H1N1 INFECTION
The primary complication with new H1N1 infection is profound primary influenza pneumonia, and deaths are usually related to this problem. Physicians have experienced extreme difficulty in ventilating these patients. As a result, extracorporeal membrane oxygenation—a technique that long fell out of favor in adult medicine—has renewed interest. The pneumonia is particularly a problem in infected people with preexisting cardiovascular disease or lung disease (especially asthma), pregnant women, and obese individuals. Obesity is a remarkably apparent risk with this influenza that has not been recognized in the past.
Secondary bacterial pneumonias can occur with H1N1 influenza, particularly in older people, immunocompromised individuals, and those with preexisting lung disease. Some nonpulmonary complications can be severe or fatal. People infected with H1N1 have developed rhabdomyolysis, myocarditis, and toxic shock syndrome (related to secondary bacterial, especially Group A streptococci, infections). There is concern that neurologic sequelae such as Reye syndrome may occur in children.
INFLUENZA INFECTION CONTROL AND TESTING
Transmission of this virus occurs primarily by large droplet nuclei through coughing and sneezing—some transmission may occur by fomites and respiratory aerosol. It is important to educate people to cough into their sleeve or elbow instead of their hands. Hand washing 10 times a day reduces the risk of getting influenza.1
The median incubation period is only two days. In adults, the period of infectivity occurs right before or the day before symptoms begin and lasts up to seven days after the onset of clinical illness. Children can shed virus longer and may be infectious before symptoms begin and for a while after they seem to have recovered. Immunocompromised individuals can shed virus for weeks and even months. H1N1 influenza is generally an illness of five to seven days unless a complication develops.
The rapid flu test—a functional assay that is linked in a rapid card test—which many physicians have in their clinics, has been disappointing. In some studies, only 40% of people with new H1N1 infection have a positive rapid flu test result, so physicians should not exclude that diagnosis if the neuraminidase activity assay finding is negative. The best test is the real-time polymerase chain reaction assay if it is available, or another nucleic acid-based assay.
TREATMENT
It has been argued that anyone who has a flu-like illness should be treated for H1N1, but there is concern that the drug supplies will not last. Physicians should especially treat individuals who are at greatest risk—pregnant women, immunocompromised patients, young children, patients with underlying metabolic or cardiopulmonary disease, and probably obese patients as well.
One argument to prescribe oseltamivir or other neuraminidase inhibitors is that it might decrease the period of viral shedding, assuming the virus is susceptible and patients are absorbing the medication. But from an epidemiologic perspective, it may be worthwhile to treat infected individuals to decrease their ability to transmit to others. However, that is only true if the drug is given early on—a substantial virus peak occurs even with treatment.
Two standard medications are on the market—oseltamivir (Tamiflu—Roche Laboratories), an oral preparation, and zanamivir (Relenza—GlaxoSmithKline), an inhaler. Both drugs are effective and H1N1 is susceptible to both, although resistance has been described.2 Peramivir (BioCryst Pharmaceuticals) is an intravenous formulation now available on a compassionate-use basis for some severely ill individuals in which an intravenous route is preferred.
These antivirals need to be administered as early in the infection process as possible, and a negative rapid flu test result should not exclude the diagnosis. Infected individuals should not wait to see what happens before filling their prescriptions. These individuals should be socially isolated. If they get sick, they should see their physician again within a couple of days because they may be developing a complication such as primary influenza pneumonia or a secondary bacterial pneumonia, or they may have a neuraminidase-resistant organism. And, in my opinion, physicians should make an assessment from a public health perspective regarding what is occurring with the rest of the family. For example, the infected individual's pregnant wife or 3-month-old baby at home should be of great concern. Physicians should make efforts to treat not only the patient but also their at-risk close contacts to prevent illness in the family.
VACCINATION
Inactivated and live-attenuated vaccines against new H1N1 are available. These vaccines were made by using the same manufacturing system we have been using for the seasonal influenza vaccines for decades—nonadjuvanted, basic chick-embryo-based, safe vaccines.
Physicians should apply the same dos and don'ts regarding who should and should not receive this vaccine as they do with the seasonal influenza vaccine. The only caveat is that if a patient received the live-attenuated seasonal influenza vaccine, physicians must wait at least four weeks to administer the monovalent, inactivated new H1N1 vaccine. Otherwise data suggest the same type of side effect profile as seen with the standard seasonal influenza vaccine can occur.
The priority groups for vaccination are pregnant women, followed by young children, then older children, and then the caregivers of children less than 6 months old (who cannot receive the vaccine). The next priority groups are police officers, firemen, public health authorities, healthcare workers, and, finally, adults with one of the risk factors for severe influenza.
FINAL THOUGHTS
Since this is a current event, we do not know how it will unfold over the winter months. However, we can make a few predictions based on what happened in the southern hemisphere. It has been bad, but it could be a lot worse.
What could be worse? Antiviral resistance could spread, or mutational events could increase the intrinsic virulence of the organism. A hybrid H5N1-new H1N1 virus would be particularly unpleasant. There may be additional delays in vaccine manufacturing, or it may turn out that the vaccine does not work as well as we think it is going to work. Antiviral drug stocks may become depleted (which has not happened). Or we could have a second hit—this pandemic influenza followed in the same year by another respiratory virus.
As healthcare workers, we have to stick together and try to protect as many people as we can and rethink our approach to the next pandemic. The public health response to this outbreak has been disappointing, and we can and should do better in the future.
Speaker: Steven Opal, MD
Division of Biology and Medicine
Alpert Medical School
Brown University
Providence, RI 02912
Dr. Opal presented this information at the physician and veterinarian collaborative seminar "Pets, People, and Pathogens: Emerging Diseases" on November 18, 2009, in Providence, R.I. Coastal Medical (Providence, R.I.) and the Companion Animal Parasite Council jointly sponsored this seminar.
Special thanks to Theresa Entriken, DVM, for writing this lecture summary and sharing this information with Veterinary Medicine readers.
REFERENCES
1. Mitka M. Hand washing, a key anti-flu strategy, often neglected by health care workers. J Am Med Assoc 2009;302(17):1850-1851.
2. Chen H, Cheung CL, Tai H, et al. Oseltamivir-resistant influenza A pandemic (H1N1) 2009 virus, Hong Kong, China. Emerg Infect Dis 2009;15(12):1970-1972.
UN, WHO address public health concern over avian flu transmission to humans
April 18th 2024Veterinary professionals working with certain animals are advised to take precautionary steps to minimize risk of infection, while researchers in Texas study potential H5N1 vaccines, antivirals, and antibody therapies for humans
Read More
UN, WHO address public health concern over avian flu transmission to humans
April 18th 2024Veterinary professionals working with certain animals are advised to take precautionary steps to minimize risk of infection, while researchers in Texas study potential H5N1 vaccines, antivirals, and antibody therapies for humans
Read More
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.