Why three is better than two: An overview of three- vs. two-view thoracic radiographic studies
Untitled Document
Next >
Radiographic examination of the thoracic cavity has typically consisted of a minimum of two orthogonal views, usually left or right lateral and ventrodorsal (VD) or dorsoventral (DV). The other lateral view may have been omitted because of the owner’s finances, a lack of time, a lack of patient cooperation, the instability of the patient’s health, or a concern for patient and human radiation exposure.
Nevertheless, studies have shown that important findings within a patient’s thoracic cavity have been missed when only two views were evaluated.1,2 Because of this potential to miss findings, we recommend practitioners consider three-view thoracic radiographic studies (left and right lateral recumbent views and a ventrodorsal or dorsoventral view) as the routine standard of care.
PATIENT POSITIONING
To maximize the diagnostic value of radiography, proper patient positioning is essential. A key element to ensure proper positioning is removing all extraneous material, including collars, leashes, bandages, and any blood, water, or dirt from the patient’s skin or fur. Depending on the patient’s health status and level of cooperation, physical or chemical restraints may be used to obtain the radiographs. To minimize human radiation exposure, items such as sandbags or tape can be used to restrain and position a patient.3
Lateral positioning
For lateral thoracic radiographs (Figure 1A), pull the forelimbs cranially as far as possible so they are not superimposed over the cranial thorax or cranial margin of the heart, which can obscure underlying abnormalities. The radiograph should extend from the shoulder to the dorsal aspect of the diaphragm so the field of view extends from the thoracic inlet to the caudodorsal lung field. The heads of the ribs should be superimposed.
Take the radiograph during peak inspiration to achieve maximum contrast between the air-filled lung and potential soft tissue opacity disease, such as pneumonia, primary neoplasia, or metastatic disease. You can identify peak inspiration by noting the caudodorsal region of the caudal lung lobes extending caudal to T12, the cranial margin of the left cranial lung lobe extending to the level of the first rib, increased aeration of the accessory lung lobe, and the cardiac silhouette separated from the diaphragm.3-5
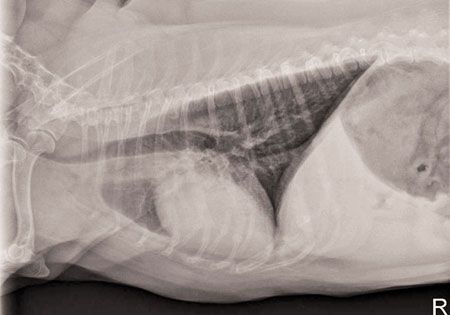
Figure 1A: This canine right lateral thoracic radiograph illustrates appropriate patient positioning. The field of view extends from the thoracic inlet to the caudodorsal lung fields. The forelimbs are pulled cranially so they are not superimposed over the cranial thorax or cranial margin of the heart. The rib heads are superimposed. (All photos courtesy of Drs. Cynthia Strelec and William Lee.)
Ventrodorsal or dorsoventral positioning
For ventrodorsal or dorsoventral radiographs (Figure 1B), pull the forelimbs cranially as indicated for a lateral radiograph. When a lesion is suspected in the cranial lung lobes on the ventrodorsal or dorsoventral view, the forelimbs could be pulled caudally to rotate the scapulae away from the cranial thorax to improve visualization of these lobes. The sternum should be superimposed over the spine along the entire length of the thorax.
The field of view should extend from the level of the shoulder joint to the last rib in order to include the thoracic inlet and allow full evaluation of the lungs during peak inspiration.
Radiographic findings indicative of peak inspiration include the caudolateral region of the caudal lung lobes extending caudal to T10, the diaphragm cupola being caudal to the mid-T8 vertebral body, and increased thoracic cavity width and length.3-5
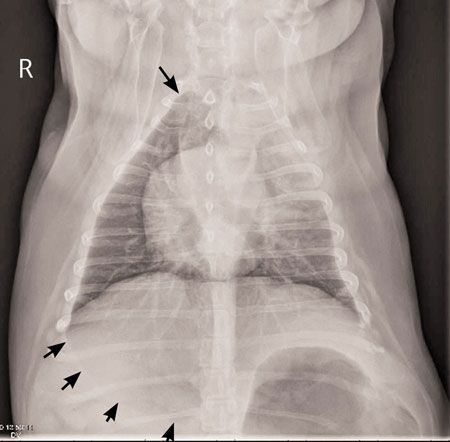
Figure 1B: This canine dorsoventral thoracic radiograph illustrates appropriate patient positioning. The forelimbs are pulled cranially so they are not superimposed over the cranial thorax. The field of view extends from the thoracic inlet to the caudal aspect of the rib cage to include the cranial (top arrow) and caudal (bottom arrows) lung margins. The sternum is positioned over the spine.
RADIOGRAPHIC TECHNIQUE
Selecting the proper technique (kVp and mAs) is essential, otherwise poor radiographic quality due to underexposure or overexposure may lead to misinterpretation and misdiagnosis of disease. Record the individual patient settings so the same technique can be used when follow-up radiographs are taken to allow for more critical evaluation of the disease progression.3,4
WHAT TO LOOK FOR
Pulmonary disease
The effect of patient positioning must be understood in order to evaluate the thoracic cavity for disease and appreciate the necessity for incorporating three-view studies as the standard of care in practice. Distinct differences between left and right lateral thoracic radiographs are evident, especially when evaluating patients for pulmonary disease.
Studies have demonstrated that when patients are in lateral recumbency, the dependent lung is partially collapsed because of gravity and compression by the heart. As a result, the dependent lung has a reduced volume of air and increased radiopacity.
Thus, a pulmonary lesion that has soft tissue opacity and is located in the dependent lung will silhouette with the increased opacity of the surrounding lung tissue and may not be detected. When a soft tissue opacity pulmonary lesion is located in the nondependent lung, it can be detected because of contrast with the air in the fully expanded lung.6
Differences in ventrodorsal and dorsoventral views are important to recall when evaluating this same patient for pulmonary disease. The accessory lung lobe region is more visible in the ventrodorsal view than in the dorsoventral view, where it is less aerated because of the cranial displacement of the diaphragm. The dorsoventral view is preferred for evaluating soft tissue opacity lesions in the caudodorsal lungs because of better inflation of the caudodorsal lungs in sternal recumbency. Conversely, pulmonary lesions of gas opacity (e.g. bullae) may be better detected in the dependent, partially collapsed lung.3,7
When a patient is being evaluated for pulmonary disease (e.g. primary neoplasia, metastatic disease, infiltrative disease, pneumonia), obtaining left and right lateral recumbent and ventrodorsal or dorsoventral thoracic radiographs is necessary because important lung lesions may not be detected if all three views are not evaluated (Figures 2A-2C).2,3,5,7-10
In one study, a change in diagnosis would have been made in 12% to 15% of patients that were evaluated for possible structural interstitial pulmonary disease, including metastatic neoplasia, when three-view (left and right lateral views and a ventrodorsal view) thoracic studies were available compared with only two-view thoracic studies (right or left lateral views and a ventrodorsal view).9
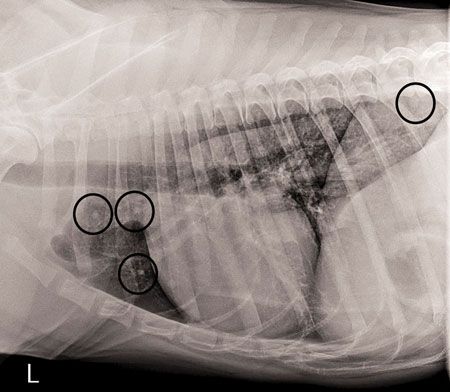
Figure 2A: This canine left lateral thoracic radiograph shows evidence of metastatic neoplasia (circles).
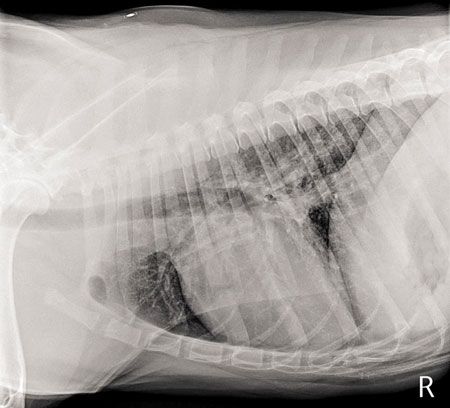
Figure 2B: This canine right lateral thoracic radiograph shows no evidence of the metastatic neoplasia seen in Figure 2A of the same patient.
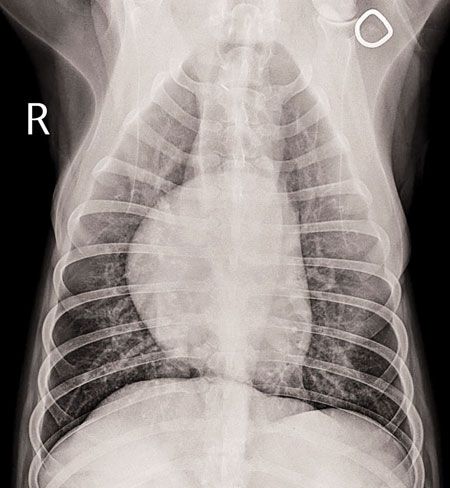
Figure 2C: This canine ventrodorsal thoracic radiograph shows no evidence of the metastatic neoplasia seen in Figure 2A of the same patient.
Cardiac silhouette and pulmonary vasculature
Distinct differences in the cardiac silhouettes of left and right lateral thoracic radiographs support the evaluation of both lateral views in a thoracic study, along with a ventrodorsal or dorsoventral view.
On the right lateral view, the cardiac silhouette is oval-shaped and in contact with the sternum (Figure 3A). On the left lateral view, the cardiac silhouette has a rounded shape and is in less contact with the sternum (Figure 3B). If not carefully evaluated, this cardiac silhouette could be misdiagnosed as right ventricular hypertrophy because of the heart’s shape or as a pneumothorax because of its apex being elevated from the sternum.
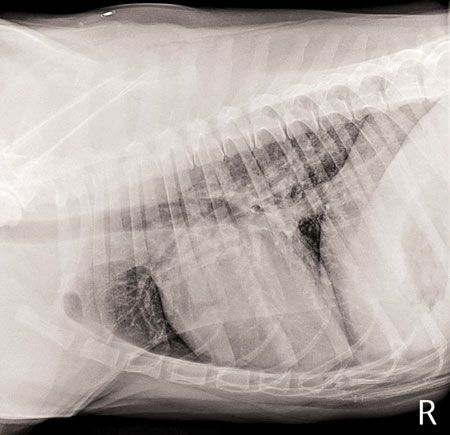
Figure 3A: In this canine right lateral thoracic radiograph, the cardiac silhouette is oval-shaped and in contact with the sternum.
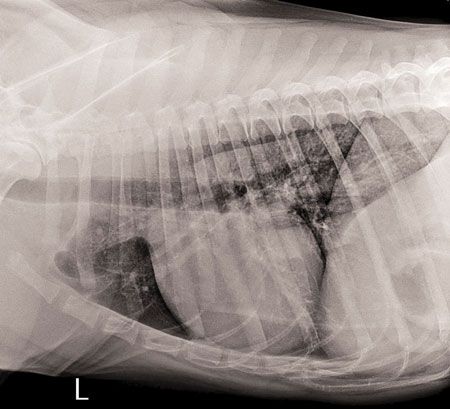
Figure 3B: In this canine left lateral thoracic radiograph, the cardiac silhouette is rounded and in decreased contact with the sternum.
The dorsoventral view allows for better evaluation of the cardiac base because the cardiac silhouette appears elongated on the ventrodorsal view (Figures 4A & 4B). Compared with the ventrodorsal view, the position of the cardiac silhouette on the dorsoventral view is less dependent on the conformation of the thoracic cavity.1,3-5
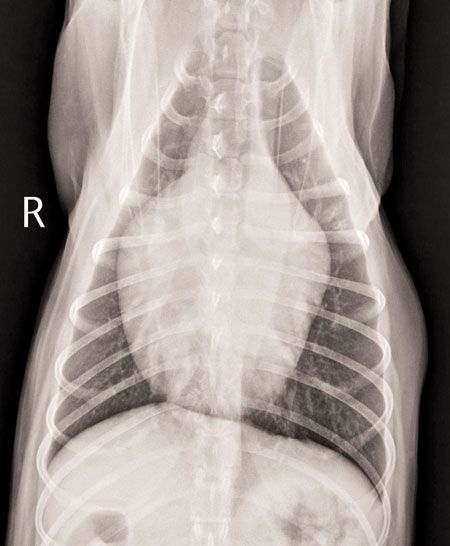
Figure 4A: This canine ventrodorsal thoracic radiograph illustrates elongation of the cardiac silhouette when compared with Figure 4B of the same patient.
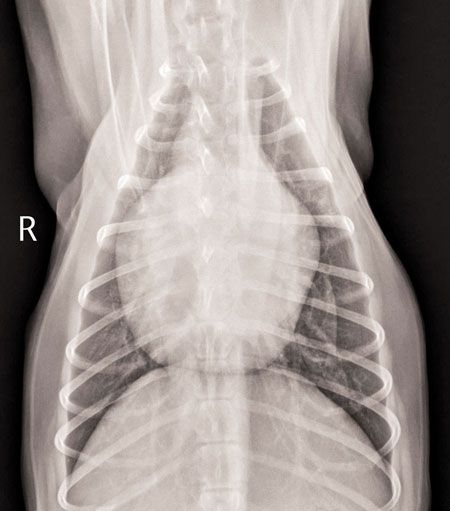
Figure 4B: This canine dorsoventral thoracic radiograph illustrates the difference in appearance of the cardiac silhouette and cardiac base from the ventrodorsal view of the same patient as in Figure 4A.
The pulmonary vasculature has distinct differences on lateral, ventrodorsal, and dorsoventral views. The left lateral view provides better separation of the left and right cranial lobar arteries and veins (Figure 5A). The left and right cranial lobar arteries and veins are superimposed on the right lateral view and are, thus, more difficult to evaluate (Figure 5B).
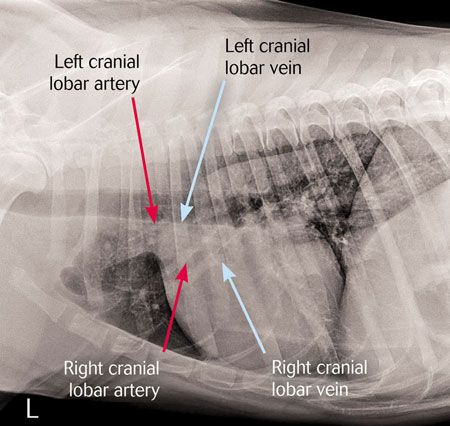
Figure 5A: This canine left lateral thoracic radiograph shows the separation of the left and right cranial lobar vessels, which aids in their evaluation.
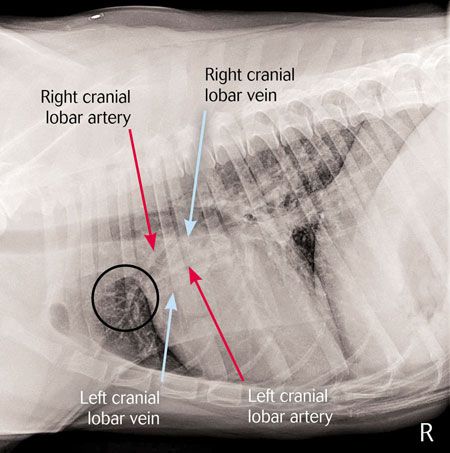
Figure 5B: This canine right lateral thoracic radiograph shows the left and right cranial lobar vessels superimposing onto one another (circle).
The dorsoventral view provides better evaluation of the caudal lobar vessels than the ventrodorsal view does because of the vessels’ magnification and more perpendicular relation to the X-ray beam. There is better aeration of the lungs in sternal recumbency (dorsoventral view), which also aids in evaluation of the caudal lobar vessels (Figures 6A & 6B). In patients with pulmonary edema, the caudodorsal lung lobes are most commonly affected, and decreased visualization of the caudodorsal pulmonary vessels can support this diagnosis.
The dorsoventral view also allows for easier assessment of the pulmonary veins, which become dilated with left-sided cardiac congestion.3-5,8,11
By incorporating three-view thoracic radiographic studies, the pulmonary vasculature can be assessed for changes, along with the entire thoracic cavity, and aid in diagnosing cardiogenic and noncardiogenic disease.
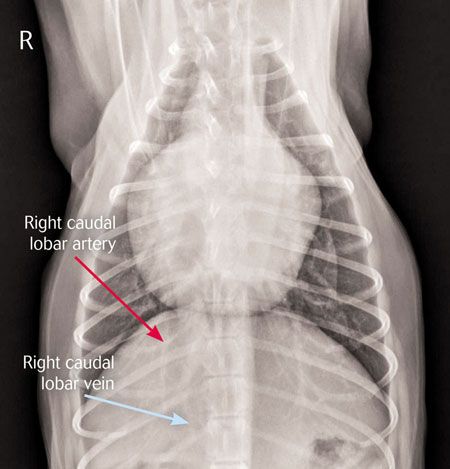
Figure 6A: This canine dorsoventral thoracic radiograph illustrates the caudal lobar vessels.

Figure 6B: This canine ventrodorsal thoracic radiograph shows decreased visibility of the caudal lobar vessels in comparison with Figure 6A of the same patient.
Pleural effusion
In patients with suspected pleural effusion, the lateral views are helpful to detect pleural fissure lines, which are the result of the separation of lung lobes from the thoracic wall and adjacent lobes. The pleural fissure lines are seen radiographically as linear soft tissue opacities at the anatomic locations corresponding to interlobar fissures.3,5
Studies have revealed that the ventrodorsal view is preferred for evaluating cranial and right middle lung lobes, the cranial mediastinum, and the size and shape of the cardiac silhouette in patients with pleural effusion because the fluid is distributed over a larger area in the dorsal thoracic cavity and is less likely to obscure these structures.3-5,11 Small-volume pleural effusions are more visible as pleural fissure lines on the ventrodorsal view than on the dorsoventral view, in which the small-volume pleural effusion collects dorsal to the sternum and does not enter the interlobar fissures.3-5,11
The dorsoventral view provides better visualization of the caudal lung lobes, major pulmonary vessels, and hilar structures; the cardiac silhouette will be obscured by the ventral distribution of the pleural fluid. Depending on the patient’s stability, a dorsoventral view may be better tolerated than a ventrodorsal view because ventrodorsal positioning can compromise respiration. Consider patient stabilization and thoracocentesis before obtaining radiographs.3-5,11
Pneumothorax
With the presence of gas in the pleural space, lung retraction from the thoracic wall can be radiographically detected on lateral, ventrodorsal, and dorsoventral views.3 Based on previous studies, specific views have been recommended for patients with a suspected pneumothorax.
Vertical beam left lateral recumbent and expiratory horizontal beam ventrodorsal views were most effective in detecting pneumothorax because of the dorsal elevation of the heart from the sternum and the apex of the heart shifting toward the lower lung, which is not expanding.3,12 Studies revealed that the cardiac silhouette was dorsally displaced from the sternum on the vertical beam left lateral view with greater consistency than with the right lateral view.12
The dorsoventral view is more sensitive in detecting a pneumothorax than the ventrodorsal view because of increased radiopacity of the lung parenchyma, clearer lung lobe margins, and no evidence of the pulmonary vessels crossing the lung lobe margins. Also positioning and restraining patients with a pneumothorax in sternal recumbency for the dorsoventral view is less stressful than positioning and restraining them in dorsal recumbency for a ventrodorsal view.3,13
In a recent study, it was concluded that horizontal beam projections aided in the diagnosis of pneumothorax when used with standard vertical beam projections.14 Right and left lateral horizontal beam ventrodorsal projections and the standard vertical beam left lateral projection were more likely to detect and grade pneumothorax severity than the vertical beam dorsoventral and ventrodorsal views were. The right lateral horizontal beam projection had the highest rate of detection and gradation of severity for pneumothorax. Dorsoventral and ventrodorsal projections had the lowest sensitivity for detection of pneumothorax and lowest gradation of severity for pneumothorax because of skin folds being misdiagnosed as a pneumothorax and the decreased visibility of the retracted caudal lung lobes, as a result of the superimposed ribs, aorta, diaphragm, and stomach.14
The misdiagnosis of pneumothorax has been documented in ventrodorsal and dorsoventral views.3,15 Chondrodystrophic breeds that are rotated on a ventrodorsal or dorsoventral view have been misdiagnosed with pneumothorax because of the radiolucent periphery of the thoracic cavity.3 Skin folds have resembled the appearance of a lung retraction and created a linear opacity that extended caudally past the margin of the pleural space and superimposed over the diaphragm.15
The horizontal beam projection is recommended to determine whether a pneumothorax is present or whether the radiographic findings were due to a skin fold or patient positioning.
CONCLUSION
Incorporating three-view thoracic radiographic studies (left and right lateral recumbent views and a ventrodorsal or dorsoventral view or horizontal beam view when pneumothorax is suspected) as the routine standard of care in practice will assist in the thorough evaluation of a patient’s thoracic cavity for possible disease and structural abnormalities. Without three-view thoracic radiographic studies, there is the potential for missing important findings or misdiagnosing diseases and, thus, misinforming owners and not meeting the needs of patients.