Aggressive vs. palliative: Veterinary decision trees for pet cancer
These basic algorithms provide every veterinarian a framework for diagnosing cancer and deciding with pet owners on the right course of treatment for a cure, a longer life or improved quality of life.
Surgery, radiation therapy and chemotherapy-the mainstays of cancer treatment in pets-can confer significant benefit to cancer patients. However, they are equally capable of producing significant morbidity if used without discretion. Your two key questions are these: “What benefits can a patient derive from cancer therapy?” and “How do you judge whether a patient is likely to experience these benefits?”
What do we hope for?
To address the first question, let's look at the three fundamental ways cancer patients benefit from therapy:
1) The pet's cancer is cured
2) The pet's life is extended in the absence of cure, while quality of life is concomitantly maintained or improved
3) The pet's quality of life is improved in the absence of cure or extension of life.
To achieve a cure in patients with advanced cancers, aggressive therapy is usually required. With aggressive therapy comes a significant risk of treatment-related complications. In contrast, treatments with more palliative intent frequently improve quality of life and may also extend life if used carefully. It should be noted that the use of the term “palliative” here is not synonymous with hospice-style care for a terminally ill patient. Radiation therapy, chemotherapy and even surgery all can be used with palliative intent. However, as opposed to the rationale for their use in the aggressive treatment setting, the focus of palliative therapy is to minimize treatment-related morbidity. This necessarily comes at some expense to the prospects of curing a cancer or extending a patient's life.
Can it happen?
Fully answering the question of how to judge whether a patient is likely to derive benefit from therapy requires some review of the typical diagnostic and staging process for cancer patients …
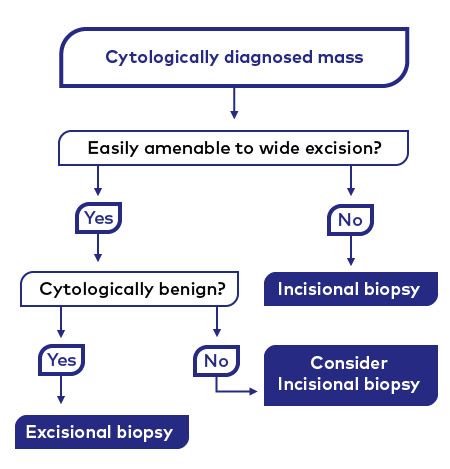
Figure 1, a decision tree on collection of biopsy specimens from tumors. The purpose of biopsy is to obtain histopathologic confirmation of the tumor type and, where applicable, tumor grade. A decision central to this process is whether incisional or excisional biopsy is the most appropriate choice for a given tumor (see Figures 2 and 3). Note that incisional biopsy is still potentially useful for tumors amenable to wide excision. Here, it may provide information about the tumor's biological aggressiveness, which may sway a pet owner's decision to comply with your recommendation for curative-intent surgery.
> Cytologically diagnosed mass. Figure 1 details the initial decision-making process for a patient with a newly diagnosed tumor, assuming that the tumor has been sampled by fine-needle aspirate cytology. If cytology suggests cancer, then collecting a biopsy samples for histopathologic confirmation of this diagnosis is of paramount importance. Ideally, the biopsy should also define the cancer grade (how malignant the tumor's behavior is likely to be). Low-grade tumors tend to grow slowly and metastasize with reluctance, and are curable with wide surgical excision. High-grade tumors, in contrast, grow rapidly and metastasize readily, and are rarely curable even with aggressive surgical excision.

Figure 2. This low-grade cutaneous mast cell tumor makes this dog a candidate for excisional biopsy. This tumor, measuring approximately 1 cm in maximal diameter, is confined to the dermis and located over the lateral thorax. The dog owner noticed that it grew slowly to this size over many months. The size, depth of extension, and anatomic location make the tumor amenable to wide surgical excision. These features, along with the slow growth rate, further suggest a benign biological behavior. Collectively, these characteristics support the tumor's suitability for excisional biopsy. (Photo courtesy of Dr. Michael Childress)
When planning a biopsy, the clinician must decide whether to remove the tumor entirely via excisional biopsy or to perform an incisional biopsy and wait for the histopathology results before planning definitive therapy. An example of a tumor suitable for excisional biopsy is presented in Figure 2, while a tumor for which incisional biopsy may be more appropriate is presented in Figure 3.

Figure 3. This high-grade cutaneous mast cell tumor makes this dog a candidate for incisional biopsy. This tumor, measuring approximately 4 cm in maximal diameter, is palpably invasive to the subcutis and located over the caudal thigh, lateral to the vulva. The dog owner noticed that it grew rapidly over the past several weeks. It has an ulcerated surface, implying an aggressive biological behavior. As such, extensive surgical resection is likely necessary to provide durable local tumor control. However, the proximity to the vulva and depth of invasion will limit the extent of surgery that can be performed. Because the tumor may be aggressive and local control may be difficult to achieve surgically, incisional biopsy is indicated prior to planning definitive therapy. (Photo courtesy of Dr. Michael Childress)Although pet owners may balk at the added expense of incisional biopsy, poorly planned excisional biopsies can lead to such serious complications as wound dehiscence and tumor recurrence. In patients in which an aggressive cancer is suspected, an incisional biopsy can provide valuable information as to what types of benefit (see above) may be derived from therapy as well as the extent of treatment necessary to achieve these outcomes. Many pet owners may, quite reasonably, forego surgical tumor removal if an incisional biopsy suggests the pet's prognosis for survival is poor.

Figure 4, a decision tree for initial choices between aggressive and palliative therapy a tumor. This is based on tumor stage and the patient's overall health. Healthy patients with low-stage cancers are the most appropriate candidates for aggressive therapy, while unhealthy patients with advanced-stage disease are candidates for palliative therapy.
> Histologically confirmed cancer. When clients wish to pursue cancer treatment for a pet after a biopsy diagnosis, staging tests should be ordered to determine the extent of its cancer and its ability to tolerate therapy (Figure 4). The staging process typically consists of a battery of diagnostic imaging studies to estimate the primary tumor's size and to screen for metastatic lesions. Laboratory tests typically are also performed to gauge the pet's overall health. Pets with no serious comorbid disease, resectable primary tumors and no evidence of metastatic disease are the best candidates for aggressive cancer therapy. Pets who don't meet these criteria should be considered more appropriate for palliative treatments.
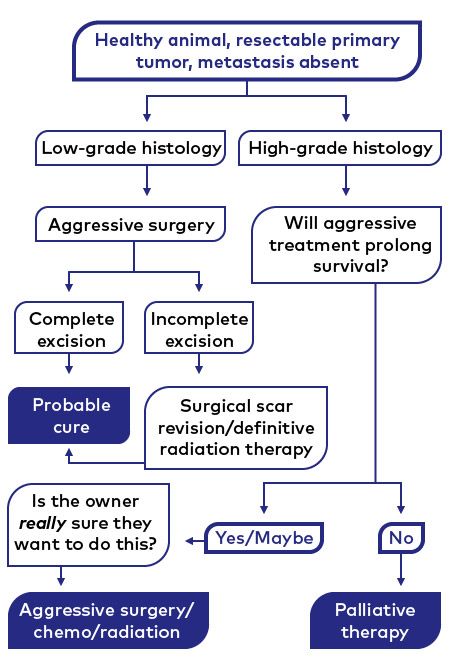
Figure 5, a decision tree on final decisions between aggressive and palliative therapy for a tumor. For healthy patients with low-stage tumors, the decision to pursue aggressive therapy is further dictated by the histopathologic tumor type and grade. Indolent, low-grade tumors have the best chance to be cured by aggressive therapy. Aggressive, high-grade tumors may benefit from aggressive therapy, but are unlikely to be cured. Clear communication with pet owners on the goals of therapy is an essential prerequisite to pursuing aggressive treatment in patients with high-grade tumors. Since aggressive therapy may not extend survival and may produce serious side effects, palliative therapy may be a better option for many of these patients.
> A healthy animal with a resectable primary tumor and metastasis absent. The final decision to pursue or forego aggressive cancer therapy takes information from both the tumor biopsy and the staging process into account (Figure 5). Animals with low-grade, resectable, nonmetastatic tumors are ideal candidates for aggressive cancer surgery and are often cured of their cancers.
In contrast, animals with high-grade tumors are considerably less likely to be cured, even with aggressive, multimodal therapy. For these patients, the key question is, “Can aggressive therapy extend their lives to a greater extent than would be possible with palliative therapy?” For most high-grade cancers, aggressive therapy has yet to a show a clear survival advantage over palliative therapy. While an aggressive approach may still benefit some patients with these cancers, the decision to pursue aggressive therapy should only be made after careful discussion with your client.
With these principles in mind, usually it's possible to generate a treatment plan for pets with cancer that balances clinical benefit with treatment-related morbidity. Striking this balance is critical to affording a satisfactory outcome from treatment to both the patient and the pet owner. Moreover, it also honors that time-tested medical aphorism: Never make the treatment worse than the disease.
Michael O. Childress, DVM, MS, DACVIM (Oncology), is associate professor of comparative oncology at Purdue College of Veterinary Medicine.