A challenging case: Primary hyperparathyroidism in a dog
An 8-year-old 50.6-lb (23-kg) neutered male Airedale terrier was presented to Forest Hill Animal Clinic for a wellness examination and laboratory tests.
An 8-year-old 50.6-lb (23-kg) neutered male Airedale terrier was presented to Forest Hill Animal Clinic for a wellness examination and laboratory tests. The dog was receiving levothyroxine (300 µg orally every 12 hours) for previously diagnosed hypothyroidism, and tylosin (200 mg orally every 12 hours) and Prescription Diet i/d Canine (Hill's Pet Nutrition) for chronic colitis of four years' duration. The dog also had a history of chronic arthritis and had received meloxicam in the past.

Vital Stats
HISTORY
Five months before the wellness examination, the dog had been presented to a veterinary emergency clinic for evaluation of lethargy of one day's duration. The dog's vital signs were normal. An electrocardiogram (ECG) had been obtained, and the results were normal. A serum chemistry profile had revealed that the total calcium concentration was 3.1 mmol/L (reference range = 2.2 to 3 mmol/L). The albumin concentration was normal. The parathyroid hormone (PTH) concentration had been measured because of the increased calcium concentration, and it was normal (3.9 pmol/L; reference range = 3 to 17 pmol/L). The patient had been discharged 48 hours after receiving intravenous fluid therapy and supportive care.
PHYSICAL EXAMINATION AND LABORATORY FINDINGS
A physical examination at Forest Hill Animal Clinic revealed mild dander, a dry coat, and ceruminous debris in both ears. Complete blood count (CBC) results were normal, and results of a heartworm antigen test were negative.
Further testing revealed a total calcium concentration of 3.5 mmol/L, with an ionized calcium concentration of 1.82 mmol/L (reference range = 1.25 to 1.45 mmol/L), a PTH concentration of 4 pmol/L, a nonmeasurable parathyroid hormone-related peptide (PTHrP) concentration, and a normal vitamin D concentration (120 nmol/L; reference range = 60 to 215 nmol/L).
The owner indicated that the dog had not been exposed to toxins, including vitamin D supplements or creams. The dog was then referred to a referral center in Toronto for further evaluation of persistent hypercalcemia.
REFERRAL HOSPITAL PATIENT EVALUATION
Results of another CBC and serum chemistry profile revealed a total calcium concentration of 3.5 mmol/L. The dog's free T4 concentration was normal (31.9 pmol/L; reference range = 16 to 45 pmol/L). A urinalysis revealed a specific gravity of 1.005, 10 to 20 calcium oxalate crystals/hpf, and bacteriuria. Aerobic bacterial culture of the urine was positive for Escherichia coli, which was sensitive to enrofloxacin.
Diagnostic imaging to help determine the underlying cause of the hypercalcemia was performed. Thoracic radiography revealed no abnormalities, but abdominal ultrasonography documented multiple cystic calculi and mild renal pelvic mineralization. Cervical ultrasonography to assess the parathyroid glands revealed no abnormalities.
Differential diagnoses for the dog's hypercalcemia included lymphoma, leukemia, multiple myeloma, primary hyperparathyroidism, and, less likely, excessive vitamin D consumption (because of the normal vitamin D concentration). Surgery to remove the cystic calculi was scheduled for the next day.
Abdominal exploration, cystotomy, and bone marrow biopsy
The dog was sedated with butorphanol and midazolam. Anesthesia was induced with propofol and maintained with isoflurane. An abdominal exploratory surgery and cystotomy were performed, and multiple, 3-to-4-cm, smooth, oval calculi were removed from the urinary bladder. The bladder was closed in a routine fashion. Liver, gastric, and intestinal biopsy samples were obtained for histologic examination to rule out possible underlying gastrointestinal or multicentric lymphoma. The abdomen was closed in a routine fashion.
A bone marrow core biopsy sample from the right humerus was also obtained and submitted for histologic examination to rule out occult lymphoma, leukemia, and multiple myeloma. Postoperative abdominal radiographs documented that all calculi had been removed.
Postoperative care
After surgery, the dog received famotidine (0.5 mg/kg orally once daily for seven days), enrofloxacin (5 mg/kg orally once daily for seven days), and meloxicam (0.1 mg/kg every 24 hours for seven days). The thyroxine, tylosin, and therapeutic diet were continued as previously prescribed. Recovery from surgery was uneventful, and the dog was discharged to its owners the next day. Histologic examination of the liver, gastric, intestinal, and bone marrow biopsy samples revealed no abnormalities. The cystic calculi analysis revealed calcium oxalate composition.
FOLLOW-UP EVALUATIONS
The referring practitioner monitored the dog's total calcium concentration monthly. At the three-month check, the dog's ionized calcium concentration had increased to 1.93 mmol/L. The PTH concentration was 12.2 pmol/L, and the PTHrP concentration remained undetectable.
An ultrasonographic examination of the parathyroid glands revealed a 3.6-x-3-mm mass on the right cranial parathyroid gland. The mass was hypoechoic compared with the surrounding thyroid tissue (Figure 1). The remaining three parathyroid glands appeared to have normal echotexture but were markedly smaller. Primary hyperparathyroidism was diagnosed.
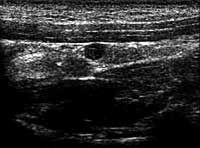
1. A sagittal ultrasonogram of the right thyroid and parathyroid glands, with the patient in dorsal recumbency. The top of the image is ventral, and the left of the image is cranial. The parathyroid adenoma is hypoechoic compared with the surrounding thyroid tissue. The diameter of the mass is 0.36 cm.
Parathyroidectomy
The next day, the dog was anesthetized as described for the cystotomy and taken to surgery for parathyroid gland exploration. Patient monitoring and intraoperative support included continuous blood pressure and ECG monitoring and pulse oximetry. A ventral cervical approach was used, and surgical dissection of the right thyroid gland revealed a 3.6-mm, round, raised mass in the cranioventral aspect of the right cranial parathyroid gland. The parathyroid glad was removed and the mass was submitted for histologic examination. The surgical site was closed in routine fashion. The dog's total calcium concentration was 3.45 mmol/L before surgery and 3.22 mmol/L six hours after surgery.
Postoperative care and outcome
After surgery, calcium carbonate was administered (1,000 mg orally every 12 hours for 14 days). On postoperative day 2, the dog's total calcium concentration was 3.05 mmol/L, and calcitriol was initiated (250 ng orally every 12 hours for 30 days) to promote intestinal absorption of calcium. On day 3, the total calcium concentration decreased to 2.73 mmol/L. On day 4, the total calcium concentration stabilized at 2.78 mmol/L, and the dog was discharged from the hospital with instructions to administer meloxicam (0.1 mg/kg every 24 hours for seven days) and continue the thyroxine and tylosin as previously prescribed.
Histologic examination of the mass was consistent with a completely excised parathyroid adenoma (Figure 2). At a follow-up examination one year later, the dog's calcium concentration was normal without calcium and calcitriol supplementation.
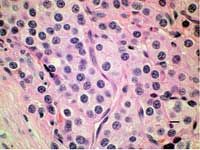
2. A photomicrograph of the parathyroid ademona (hematoxylin-eosin; bar = 10 µ).
DISCUSSION
Naturally occurring primary hyperparathyroidism is not common in dogs.1 It occurs when abnormal autonomously functioning parathyroid chief cells produce excessive PTH, most often because of a solitary adenoma.1 In one report of 72 dogs with primary hyperparathyroidism, benign adenomatous transformation of one parathyroid gland occurred in about 90% of cases, malignant transformation in 5%, and adenomatous hyperplasia in the remaining 5%.2 The condition typically affects older dogs and has no sex predilection, but Keeshonds are overrepresented and it was recently linked to a single gene with an autosomal dominant mode of inheritance.3
Clinical signs
When clinical signs develop in dogs with primary hyperparathyroidism, they tend to be mild, insidious, and nonspecific. The most common signs are polyuria, polydipsia, decreased appetite, weight loss, and lethargy. Other clinical signs frequently reported are related to cystic calculi or urinary tract infections.4
Commonly reported secondary signs related to hypercalcemia include anorexia, vomiting, and constipation. Pancreatitis is rarely observed. Mild or early disease may be nonsymptomatic and found unexpectedly on laboratory evaluation.
Diagnosis
The hallmark for primary hyperparathyroidism is persistent progressive hypercalcemia. In dogs with confirmed primary hyperparathyroidism, 102 of 187 had an initial total calcium concentration of 12 to 14 mg/dl (3 to 3.5 mmol/L).4 Hypercalcemia in conjunction with an elevated PTH concentration and an undetectable PTHrP concentration is considered the gold standard for primary hyperparathyroidism diagnosis. However, about 75% of affected dogs have normal PTH concentrations,5 which are inappropriate in the face of hypercalcemia. In normal animals, a high calcium concentration should result in undetectable PTH concentrations.
Other consistent findings on serum chemistry profiles of affected dogs include low or low-normal phosphorus, blood urea nitrogen, and creatinine concentrations. The urine is typically hyposthenuric because calcium inhibits vasopressin's action on the renal tubules. In one study, 61 of 187 dogs with primary hyperparathyroidism had a history of urolithiasis, with a large proportion of dogs initially presenting because of urinary tract signs.4
Abdominal radiography and ultrasonography identified cystic calculi in 50 of 210 dogs with primary hyperparathyroidism examined in one study.1 Abdominal imaging as well as abdominal palpation and rectal examination are also important to evaluate the abdominal organs and lymph nodes for occult neoplasia or metastasis from an anal sac adenocarcinoma. Thoracic radiography is essential in the diagnostic evaluation of dogs with hypercalcemia to identify or rule out occult neoplasia.
If no other cause of hypercalcemia is identified, a cervical ultrasonographic examination should be performed to evaluate both thyroid glands and all four parathyroid glands. Although ultrasonography results are subjective in nature, one study demonstrated a significant size difference between neoplastic (adenocarcinoma and adenoma) and hyperplastic (primary hyperplasia and secondary [renal] hyperplasia) parathyroid tissue.2 In healthy dogs, the parathyroid glands are typically
< 3 mm in diameter, while parathyroid masses are usually > 4 mm in diameter.6 Many dogs with primary hyperparathyroidism have normal or low-normal PTH concentrations, which can make diagnosis difficult, but with abnormal parathyroid ultrasonography results, the diagnosis is more likely.
Although not commonly used in veterinary medicine, radionuclide scanning of the parathyroid glands is another method to diagnose primary hyperparathyroidism.
Treatment
Treatment options for primary hyperparathyroidism include parathyroidectomy or alternative methods for ablating the affected parathyroid gland. Deciding which intervention to use should be based on lowering the risk of urolithiasis and urinary tract infections. The risk of renal failure secondary to hypercalcemia associated with primary hyperparathyroidism is reported to be low1 ; however, in a recent review of 29 dogs with primary hyperparathyroidism, renal failure was diagnosed in 24% either at presentation or up to six months after parathyroidectomy.7
Nonsurgical intervention. Nonsurgical interventions include percutaneous ultrasound-guided ethanol ablation and percutaneous ultrasound-guided radiofrequency heat ablation.8,9 Ethanol causes coagulation necrosis and vascular thrombosis within the parenchyma of the treated tissue.8 In one study, seven of eight dogs treated with ethanol (96%) injections achieved remission after the injection, with only one treatment being required in six of seven dogs and one dog requiring a second treatment to achieve complete remission.8
Percutaneous ultrasound-guided heat ablation has also been used in treating primary hyperparathyroidism in dogs.9 The main advantage of heat ablation over ethanol injection is the lowered potential to damage surrounding tissues. However, the overall outcome of one study showed that heat ablation and ethanol injection had similar remission rates.9
Surgery. Surgically removing the affected parathyroid gland, as was done in this case, is the gold standard of therapy. The most common postoperative complication is hypocalcemia because autonomous PTH production from the parathyroid tumor causes atrophy of the remaining parathyroid glands.
To help prevent hypocalcemia, maintain the total calcium concentration just below low-normal to allow the remaining parathyroid glands to regain normal PTH production. If total calcium and PTH concentrations are low after surgery, administer calcium and calcitriol to maintain calcium homeostasis until the autonomous function of the remaining parathyroid glands is restored.
Calcitriol is recommended to promote intestinal absorption of calcium, with a loading dose of 0.02 to 0.03 µg/kg (20 to 30 ng/kg) daily orally for the initial three or four days and a maintenance dose of 0.005 to 0.015 µg/kg (5 to 15 ng/kg) daily.10 Calcium supplementation can be provided by administering calcium gluconate, calcium lactate, calcium chloride, or calcium carbonate salts at 25 mg/kg orally every eight to 12 hours for four to six weeks after surgery.11
The risk of postoperative hypocalcemia correlates with the duration and severity of hypercalcemia before surgery and typically develops one to seven days after surgery.5 Because hypocalcemia can be life threatening, consider performing surgery early in the week to facilitate close monitoring of postoperative total calcium concentrations throughout the remainder of the week, unless round-the-clock care can be provided on weekends.
SUMMARY
Primary hyperparathyroidism develops infrequently in dogs, but it should remain a primary differential diagnosis in patients with persistent hypercalcemia. Although clinical signs are often vague and nonspecific, careful interpretation of total and ionized calcium, PTH, and PTHrP concentrations can help in diagnosing primary hyperparathyroidism. Cervical ultrasonography is an important diagnostic aid.
Postoperative calcium concentrations should be monitored, and oral calcium and vitamin D are often required to prevent hypocalcemia. The prognosis for dogs with parathyroid adenomas appears to be good.
ACKNOWLEDGMENTS
The author would like to thank Julie Yager, BVSc, PhD, and Susan Best, DVM, DVSc, for their excellent help with the histologic evaluation.
Michael R. Goldstein, DVM
Forest Hill Animal Clinic
1049 Eglinton Ave. W
Toronto, ON M6C 2C9
REFERENCES
1. Feldman EC, Hoar B, Pollard R, et al. Pretreatment clinical and laboratory findings in dogs with primary hyperparathyroidism: 210 cases (1987-2004). J Am Vet Med Assoc 2005;227(5);756-761.
2. Wisner ER, Penninck D, Biller DS, et al. High-resolution parathyroid sonography. Vet Radiol Ultrasound 1997;38(6):462-466.
3. Goldstein RE, Atwater DZ, Cazolli DM, et al. Inheritance, mode of inheritance, and candidate genes for primary hyperparathyroidism in Keeshonden. J Vet Intern Med 2007;21(1);199-203.
4. Ettinger SJ, Feldman EC. Disorders of the parathyroid glands. In: Textbook of veterinary internal medicine, Vol 2. 6th ed. St. Louis, Mo: Elsevier Science, 2005;1508-1535.
5. Feldman EC, Nelson RW. Hypercalcemia and primary hyperparathyroidism. In: Canine and feline endocrinology and reproduction. 3rd ed. St. Louis, Mo: Elsevier Science, 2003:661-715.
6. Wisner ER, Nyland TG, Feldman EC, et al. Ultrasonographic evaluation of the parathyroid glands in hypercalcemic dogs. Vet Radiol Ultrasound 1993;34:108-111.
7. Gear RN, Neiger R, Skelly B, et al. Primary hyperparathyroidism in 29 dogs: diagnosis, treatment, outcome and associated renal failure. J Small Anim Pract 2005;46(1):10-16.
8. Long CD, Goldstein RE, Hornof WJ, et al. Percutaneous ultrasound-guided chemical parathyroid ablation for treatment of primary hyperparathyroidism in dogs. J Am Vet Med Assoc 1999;215(2):217-221.
9. Pollard RE, Long CD, Nelson RW, et al. Percutaneous ultrasonographically guided radiofrequency heat ablation for treatment of primary hyperparathyroidism in dogs. J Am Vet Med Assoc 2001;218(7):1106-1110.
10. Chew D, Nagode L. Treatment of hypoparathyroidism. In: Bonagura JD, ed. Kirk's current veterinary therapy XIII: small animal practice. Philadelphia, Pa: WB Saunders Co, 2000;340-345.
11. Henderson AL, Mahony O. Hypoparathyroidism: treatment. Compend Contin Educ Pract Vet 2005;27(4):280-287.
Sweet pee new remedy in feline diabetes
November 9th 2023A novel class of drugs normalizes blood glucose in type 2 diabetic cats by dumping sugar into urine rather than modulating glucose uptake in the tissues but patient selection and close monitoring are crucial to using them safely
Read More