Clinical Exposures: Pulmonary thrombosis due to idiopathic main pulmonary artery disease
A 10-year-old 35.9-lb (16.3-kg) intact female Wheaton terrier was referred to the teaching hospital at Virginia Tech for evaluation of dyspnea.
A 10-year-old 35.9-lb (16.3-kg) intact female Wheaton terrier was referred to the teaching hospital at Virginia Tech for evaluation of dyspnea. The dog was accustomed to running long distances with its owner, and four days earlier the dog had run three miles. Two days after the run, the dog had collapsed after mild exercise and may have experienced a seizure. The dog had recovered from this episode within minutes, and its appetite had been normal later that day.
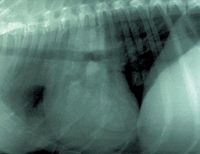
Figure 1A. The referring veterinarian obtained these thoracic radiographs when the dog was experiencing severe respiratory distress. In the lateral view (1A), the cardiac silhouette is enlarged, particularly in the cranial-caudal dimension (four intercostal spaces), and sternal contact is increased because of right ventricular enlargement. A mixed interstitial and alveolar pattern is present in the lung fields and tends to have a central distribution. The bronchi appear enlarged, and the accompanying vessels appear small.
Within the next 24 hours, the owner had noticed that the dog was having breathing difficulties and occasional coughing episodes. He took the dog to his veterinarian. The dog's vaccinations were current, and it was receiving a monthly heartworm preventive. The veterinarian's physical examination had revealed increased respiratory effort. A complete blood count had revealed a lymphopenia and a mature neutrophilia consistent with a stress response. A serum chemistry profile had revealed mildly elevated alkaline phosphatase activity (263 IU/L; normal = 0 to 140 IU/L).
The dog had been discharged from the clinic, but during the next 24 hours its respiratory signs had worsened, so the owner had returned the dog to the veterinarian. The second physical examination had revealed severe respiratory stridor with weakness and listlessness. Substantial pulmonary and cardiac abnormalities were identified on thoracic radiographs (Figures 1A & 1B). That same day, the veterinarian referred the dog to the Virginia Tech teaching hospital.
Evaluation and treatment
At Virginia Tech, physical examination revealed severe respiratory distress including dyspnea and tachypnea (60 breaths/min). The dog held its neck in extension, and the elbows were abducted. The dog's heart rate was 140 beats/min, and its rectal temperature was 98.1 F (36.7 C). On thoracic auscultation, bilateral wheezes and crackles were heard throughout the lung fields. The dog was in critical condition, so the physical examination was abbreviated, and the dog was transported to the intensive care unit (ICU).

Figure 1B. In the dorsoventral view (1B), the right ventricular silhouette is prominent (reversed D), as is the pulmonary artery segment (1- to 2-oâclock position). The middle right lung lobe and caudal part of the cranial left lung lobe have increased opacity, possibly due to pulmonary edema.
The dog was placed in an oxygen cage. Within minutes, cardiac arrest occurred, and the dog was resuscitated by administering 3.3 ml 1:1000 epinephrine intravenously and providing standard cardiopulmonary support. In addition, furosemide (1.2 mg/kg) was given intravenously for suspected pulmonary edema, and atropine (0.033 mg/kg) was given intravenously. While the dog was being prepared for echocardiography, there was a second cardiac arrest and successful resuscitation. An abbreviated echocardiographic examination, including spectral Doppler imaging, was performed in the ICU, and features compatible with pulmonary hypertension were apparent (Figure 2). Peak right ventricular systolic pressure was derived by converting the peak tricuspid regurgitant jet velocity (m/sec) to pressure by using the Bernoulli equation1 and was at least 97 mm Hg (normal = 20 to 30 mm Hg). There was no evidence of primary cardiac disease, including pulmonic stenosis. As the echocardiographic examination was being completed, cardiac arrest occurred for the third time, but efforts to resuscitate the dog were unsuccessful.
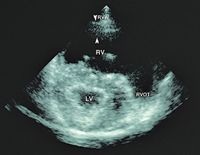
Figure 2. This echocardiogram was obtained with the dog positioned right side down and shows the heart in a right, short-axis presentation. The right ventricle (RV) is greatly enlarged by pressure and volume overload. The interventricular septum is displaced to the left, giving it a flattened appearance and causing the left ventricle (LV) to have a triangular shape. The left ventricle is smaller than normal because of the reduced pulmonary venous return to the left heart (RVW = right ventricular wall [between arrows]; RVOT = right ventricular outflow tract).
Pathologic features
A complete necropsy was performed. With the exception of hepatic lipidosis, mild membranoproliferative glomerulonephritis, and focal jejunal hemorrhage, the principal abnormalities were confined to the heart and lungs. The primary cardiac finding was an enlarged right ventricle. The pulmonary valve leaflets were normal, as was the right ventricular outflow tract. The lungs had sharply delineated areas of severe congestion, hemorrhage, and edema. These changes affected all of the right cranial and middle lung lobes as well as portions of the left cranial lobe. Thrombi were present in the arteries entering the infarcted lobes, and there was a firm and tightly adhered 1-x-0.75-cm thrombus at the junction of the main pulmonary artery and left pulmonary artery (Figure 3A). Close inspection of the main pulmonary artery surface revealed a diffuse thickening and irregularity of the intima (Figure 3A). The bulk of the thrombotic material appeared to originate at the distal limit of the abnormal intimal tissue. Histologic evaluation of the main pulmonary artery revealed extensive thickening of the intima and media due to mucin (glycosaminoglycan) deposition in these layers (Figure 3B).

Figure 3A. This necropsy specimen shows the main pulmonary artery (MPA) and a pulmonary artery (PA) branch feeding the left caudal lung lobe. The arrows define a tightly adhered pulmonary thrombus (T) at the distal limit of the main pulmonary artery. This thrombus was obstructing the artery supplying the left caudal lobe and right middle lobe. Other thrombi were noted in this region but were removed as part of the necropsy procedure. The intimal lining of the main pulmonary artery is covered with extensive deposition of irregular, raised, whitish tissue that commences just above the pulmonary valve and extends to the level of the thrombus. The pulmonary arteryâs lining appears to be grossly normal.
Discussion
Pulmonary thromboembolism is a well-recognized problem in dogs,2,3 but this case is unusual because it highlights diffuse and fatal thrombosis probably due to extensive main pulmonary artery disease. The only known similar description of this condition was reported by investigators in Sweden4 and included seven cases in Cavalier King Charles spaniels (8 to 9 years old) that died or were euthanized because of chronic valvular disease. One of the dogs had pulmonary thromboembolism, but all of the dogs had wrinkling and irregularity of the main pulmonary artery. The pulmonary valve was normal in all the dogs. The authors speculated that the abnormal main pulmonary artery tissue led to thromboembolism in the one dog and postulated that the disease in the main pulmonary artery of all seven dogs may have been related to thrombocytopenia and macrothrombocytosis. These platelet abnormalities are common in this breed.4 Furthermore, the authors pointed out that the histologic changes in the pulmonary artery wall were similar to what is seen in the cardiac valves in chronic valvular disease. They concluded that chronic valvular disease and the pulmonary artery changes might be manifestations of generalized connective tissue disease.
The subject of our report did not have any evidence of primary heart disease, including chronic valvular disease, on the basis of the history and the echocardiographic examination and necropsy findings. The platelets were not evaluated because of the nature of the presentation and the rapid demise of the animal; however, there was no evidence that this dog had clinically relevant platelet pathology.

Figure 3B. This photomicrograph shows the histologic features of the abnormal tissue in the main pulmonary artery. Mucin fills the intima (above the internal elastic membrane [IEM]) and media (below the IEM) (alcian blue-periodic acid-Schiff stain; bar = 50 µm).
This dog had pathologic evidence of glomerulonephritis, which can be associated with pulmonary thromboembolism.5 However, the histopathologic findings were mild and no hypoproteinemia was noted, so it is unlikely that glomerular disease played a role in the vascular changes or development of the thrombus in this case.
The enlargement of the right ventricle was most likely due to high right ventricular afterload. There was no evidence that this dog had turbulent blood flow that might explain the lesions in the main pulmonary artery. In addition, there was no echocardiographic or necropsy evidence of heartworms. Indeed, the owner reported that the dog had received a monthly heartworm preventive since 6 months of age. Furthermore, the normal gross appearance of the distal pulmonary arteries supports the view that heartworm disease was not involved in this animal's pulmonary problem.
This case may represent a generally unrecognized but important cause of pulmonary thrombosis in dogs. Based on the gross and histologic features, it is likely that the pulmonary vascular changes would escape clinical and echocardiographic detection until a thrombus develops. However, with improved echocardiographic capabilities, including transesophageal techniques, it may be possible in the future to identify pulmonary vascular lesions before a thrombus develops. If this were to occur, long-term antithrombotic therapy with heparin, warfarin, or aspirin might be indicated and could greatly benefit dogs with pulmonary vascular disease similar to the subject in this report.
REFERENCES
1. Kienle, R.D.: Echocardiography. Small Animal Cardiovascular Medicine (M.D. Kittleson; R.D. Kienle, eds.). Mosby, St. Louis, Mo., 1998; pp 95-117.
2. Johnson, L. et al.: Clinical characteristics of 53 dogs with Doppler-derived evidence of pulmonary hypertension: 1992-1996. J. Vet. Intern. Med. 13 (5):440-447; 1999.
3. Johnson, L.R. et al.: Pulmonary thromboembolism in 29 dogs: 1985-1995. J. Vet. Intern. Med. 13 (4):338-345; 1999.
4. Karlstam, E. et al.: Pulmonary artery lesions in cavalier King Charles spaniels. Vet. Rec. 147 (6):166-167; 2000.
5. Kittleson, M.D.: Thromboembolic disease. Small Animal Cardiovascular Medicine (M.D. Kittleson; R.D. Kienle, eds.). Mosby, St. Louis, Mo., 1998; pp 540-551.
The photographs and information for this case were provided by R. Lee Pyle, VMD, MS, DACVIM (cardiology), and Michael D. King, BVSc, Department of Small Animal Clinical Sciences; Geoffrey K. Saunders, DVM, DACVP, Department of Biomedical Sciences and Pathobiology; and David L. Panciera, DVM, DACVIM, Department of Small Animal Clinical Sciences, Virginia-Maryland Regional College of Veterinary Medicine, Virginia Tech, Blacksburg, VA 24061.