Recognizing and treating pericardial disease
Pericardial disease in small animals is relatively uncommon, but its presence may be life-threatening.
Pericardial disease in small animals is relatively uncommon, but its presence may be life-threatening. More commonly seen in dogs than in cats, the clinical signs of pericardial disease in both species can be easily overlooked or mistaken for those of other disease processes. In patients with life-threatening pericardial effusion, which has led to cardiac tamponade, it is important for you to rapidly identify and treat the elevated intrapericardial pressure. In this article, we discuss pericardial disease in dogs and cats, with a special emphasis on its diagnosis and treatment.

(Illustration by Paul Petersen)
DISEASE OVERVIEW AND CAUSES
The pericardium of dogs and cats is normally a paper-thin, translucent membrane attached at the heart base. This membrane provides the heart with a sac-like protective compartment. The normal pericardial sac contains 2 to 10 ml of clear, thin, serous fluid that acts primarily as a lubricant.1 Pericardial effusion is defined as an abnormal accumulation of fluid in the pericardial sac. If the intrapericardial pressure exceeds the pressure within the right atrium, cardiac tamponade—acute compression of the heart and impairment of ventricular filling due to increased intrapericardial pressure—may develop (Figure 1).2 When pericardial effusion is present, administering a diuretic such as furosemide will worsen the patient's cardiac output by reducing cardiac preload. Physically removing clinically significant effusions from the pericardial or pleural space as soon as possible is vital for the patient's health. In general, diuretic therapy should not be used to remove significant body cavity fluid accumulation.

1. A long-axis echocardiogram obtained from the right parasternal window in a dog. Note the marked pericardial effusion (PE) and collapse of the right atrium (RA) due to increased intrapericardial pressure. Decreased RA filling leads to reduced right ventricular (RV) filling and diminished cardiac output.
Pericardial effusion can be caused by either congenital or acquired disease. The most common etiologies are listed below in decreasing order of frequency.
Neoplasia
Cardiac neoplasia is extremely rare in cats, with lymphoma being the most common diagnosis.3 Although cardiac neoplasia in dogs is also rare, one survey of the Veterinary Medical Database reports that 0.19% of all canine tumors are cardiac, and these tumors are the most common cause of pericardial effusion in dogs.4 Hemangiosarcoma and aortic body tumors (e.g. chemodectoma) are the two most common types of tumors leading to pericardial effusion in dogs, followed by mesothelioma.4 Hemangiosarcoma is by far the most common.4
Prognosis depends on the type of tumor. Hemangiosarcomas have much more aggressive biology than aortic tumors or mesotheliomas and are likely to metastasize. Patients' mean survival time is one to three months without chemotherapy.4 Because these tumors tend to effuse more rapidly, in our experience, palliative pericardiectomy is not usually recommended for hemangiosarcoma because the risk of severe and fatal intrathoracic hemorrhage is significant.
However, in patients with aortic body tumors or mesotheliomas, tumors that effuse more slowly than do hemangiosarcomas, pericardiectomy is often palliative, allowing the fluid to be absorbed through the pleural surface and, thus, preventing the development of cardiac tamponade. Aortic body tumors are located on or surrounding the aortic arch and originate from the chemoreceptors that regulate cardiac function. These tumors are seen more commonly in brachycephalic breeds. They are typically nonresectable but slow growing and unlikely to metastasize.5 If marked pericardial effusion arises with these tumors, pericardiectomy can be palliative. In fact, one study showed that dogs with aortic body tumors treated by pericardiectomy at the time of biopsy had a median survival of 730 days, as compared with 42 days in dogs not treated with pericardiectomy.6 However, in some patients, tumor effusion is minimal and the procedure is never indicated.
Idiopathic hemorrhagic pericardial effusion
This clinical entity is second in frequency to neoplasia as a cause of pericardial effusion in dogs, reportedly accounting for 20% to 75% of cases.7 It is a diagnosis of exclusion that is arrived at after a thorough echocardiographic examination to rule out cardiac neoplasia and other possible causes of intrapericardial fluid accumulation. This disorder is more common in large- and giant-breed dogs and is thought to be an inflammatory condition affecting the pericardial sac. One-time pericardiocentesis is curative in about half of cases.8 If multiple taps are required, pericardiectomy is recommended and is usually curative.
Congestive heart failure
Although congestive heart failure is a common cause of pericardial effusion in cats, it is a less common cause in dogs.9 When congestive heart failure leads to intrapericardial fluid accumulation, cardiac tamponade is rare, and pericardiocentesis is almost never indicated.10 In some cases, however, modification of congestive heart failure medications may be warranted.
Peritoneopericardial diaphragmatic hernia
Peritoneopericardial diaphragmatic hernia (or peritoneopericardial hernia) is a congenital disorder involving anomalous development of the diaphragm and pleuropericardial membranes that allows abdominal organ herniation into the pericardial sac in dogs and cats. These rare lesions can be present for a long period without resulting in clinical signs and are occasionally diagnosed serendipitously in middle-aged patients that are presented for nonthoracic diseases. In our experience, when necessary, surgical repair of this disorder is usually successful, although the procedure is technically demanding and often requires specialized materials, such as Dacron mesh. Adult, asymptomatic animals with a peritoneopericardial hernia require no treatment, but patients with clinical signs compatible with intestinal or gastric obstruction or vascular compromise must be treated aggressively.11 Pericardial effusion is rarely present with these lesions, and, therefore, clinical signs associated with cardiac tamponade are not typical.
Left atrial rupture
In some patients with chronic mitral valve disease and severe left atrial enlargement, left atrial tearing is a possible cause of pericardial effusion. The hemorrhage rapidly leads to cardiac tamponade, cardiogenic shock, and possibly death. The pericardial effusion may contain a clot because hemorrhage is acute. The clot is often visible on an echocardiogram as a hypoechoic structure within the fluid-filled (anechoic) pericardial space. Left atrial rupture in association with degenerative mitral valve disease is apparently more frequent in male poodles, dachshunds, and cocker spaniels.12 However, any dog with severe degenerative mitral valve disease is at risk for this catastrophic sequela.12 Therefore, small-breed dogs with pericardial effusion and systolic cardiac murmurs should be evaluated critically for possible left atrial tears. Pericardiocentesis in these patients may encourage continued bleeding into the pericardial space. Therefore, in general, pericardiocentesis is not recommended in these patients. Instead, supportive care with fluid therapy and echocardiographic monitoring of effusion accumulation are preferred. If the patient destabilizes because of cardiac tamponade, pericardiocentesis is performed, but the prognosis is guarded at best.
Constrictive pericarditis
This rare disorder occurs as a result of the thickening and decreased pliability of the pericardium. The thickened pericardium causes decreased diastolic filling and clinical signs of right heart failure due to elevated right atrial pressure. This is then reflected to the systemic veins, although the pericardial effusion may be minimal. Constrictive pericarditis is extremely challenging to confirm and often requires cardiac catheterization for definitive diagnosis. Infectious etiologies (e.g. fungal infection) have been demonstrated, although the last major survey showed that most cases were idiopathic.13
Septic pericarditis
Septic pericarditis is rarely diagnosed in small animals, but dogs and cats occasionally develop infective pericarditis secondary to bacterial or fungal infections. Feline infectious peritonitis can also lead to clinically significant pericardial effusion in cats. There have been reports of sterile pericardial effusion in cats with chronic uremia, but this is uncommon.9,14
CLINICAL SIGNS
The most common, clinically significant pericardial diseases in small animals result in pericardial effusion, and it is the effusion that often leads to the clinical signs recognized by owners and practitioners. As pericardial effusion accumulates, intrapericardial pressure may exceed the diastolic right atrial and ventricular pressure. When this occurs, there may be diastolic right atrial and ventricular collapse, and right heart filling is inhibited. Because cardiac output is reduced, sympathetic tone increases and sinus tachycardia results. If the process is chronic, the renin-angiotensin-aldosterone system will be activated and will result in sodium and water retention by the kidneys. However, these mechanisms cannot compensate adequately if the elevated intrapericardial pressure is not corrected. When acute cardiac tamponade occurs, clinical signs consistent with low cardiac output often develop. Typical signs include lethargy, collapse, exercise intolerance, syncope, tachycardia, poor pulse quality, and hypotension.15 Rapid accumulation of even small volumes of fluid, as seen with hemopericardium secondary to right atrial hemangiosarcoma, can quickly lead to decompensation. This is because the pericardial membrane does not have time to stretch and intrapericardial pressure rises rapidly.1 However, the pericardium will hypertrophy and stretch over time so that patients with a slower, more gradual accumulation of fluid can often tolerate large volumes of pericardial effusion before cardiac tamponade develops. In these chronic cases, signs of volume overload, such as ascites, will be present. Because cardiac tamponade inhibits right atrial filling, elevated systemic venous pressure leads to engorged systemic veins. Cardiac tamponade and, therefore, most of these clinical signs, rarely occur in cats.16
Pulses are usually weak, and pulsus paradoxus may be present if cardiac tamponade is present. Pulsus paradoxus is an increase in pulse pressure on expiration and a decrease on inspiration.17 Although this variation in pulse strength is normally present during the respiratory cycle, pulsus paradoxus is an accentuation of this phenomenon in patients with tamponade, so much so that the variation is palpable.
Muffled cardiac sounds and a decreased palpable precordial impulse are often noted with marked volumes of pericardial fluid. Patients with cardiac tamponade and clinical signs of right heart failure usually have noticeable jugular vein distention. Sinus tachycardia is often seen as a compensatory mechanism for decreased left ventricular stroke volume in patients with cardiac tamponade due to elevated sympathetic tone.
Clinical signs specific to peritoneopericardial diaphragmatic hernias can be vague and are usually referable to the organ that is herniated. Gastrointestinal signs predominate and include vomiting, anorexia, and diarrhea, but cough and dyspnea may also be present. Patients with this type of hernia rarely present in congestive heart failure or cardiac tamponade, and the problem is most often an incidental finding on thoracic radiographs.18
DIAGNOSIS
A thorough physical examination is usually adequate to make a tentative diagnosis when cardiac tamponade is present. However, many animals with pericardial effusion have no clinical signs, and some forms of pericardial disease (e.g. peritoneopericardial diaphragmatic hernia) are clinically silent. You can use the following diagnostic modalities to confirm a tentative diagnosis of pericardial effusion before you perform pericardiocentesis. However, if a patient is clinically unstable, you may not have enough time to perform all of these tests before doing a pericardiocentesis.
Electrocardiogram
Electrocardiogram (ECG) findings can support a diagnosis if a marked volume of pericardial effusion is present, but ECG findings are not pathognomonic. Electrocardiographic findings consistent with a diagnosis of pericardial effusion include
1. Decreased R-wave amplitude (due to increased fluid insulation between the heart and surface electrodes)
2. Sinus tachycardia (with concurrent cardiac tamponade)
3. Electrical alternans, particularly when large volumes of effusion are present. This is the phenomenon in which the R-wave amplitude varies markedly in a beat-to-beat fashion (Figure 2).19 Electrical alternans, produced by swinging of the heart within the fluid-filled pericardial space, is usually only present with large effusions. It has been shown in an experimental model that electrical alternans is rate-dependent and is most likely to occur at relatively normal heart rates in dogs (90 to 144 beats/min).20
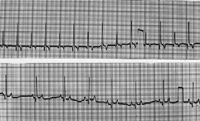
2. These lead II ECGs (25 mm/sec) from a dog show electrical alternans in the top image and a sinus rhythm without electrical alternans after pericardiocentesis in the bottom image. Note the reduction in heart rate after pericardiocentesis.
4. Ventricular complexes may also be present.
With pericardial abnormalities such as peritoneopericardial diaphragmatic hernias, the ECG findings may be normal.
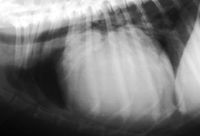
3 & 4. Lateral and dorsoventral thoracic radiographs from a dog with marked pericardial effusion. Note the large, round or globoid cardiac silhouette typical with large amounts of pericardial effusion.
Thoracic radiographs
High-quality thoracic radiographs are invaluable for diagnosing pericardial effusion and usually demonstrate a globoid cardiac silhouette. The size of the cardiac silhouette will depend on the volume of effusion (Figures 3 & 4). Pericardial effusion can often be distinguished from dilated cardiomyopathy because the cardiac silhouette is rounder and more clearly demarcated. However, you must consider other possible differential diagnoses for a large, rounded cardiac silhouette, such as tricuspid dysplasia. Also, occasionally small effusions can lead to cardiac tamponade, yet the radiographic findings are ambiguous. Rarely, heart base tumors can be seen on radiographs; they may lead to tracheal deviation.

Ultrasonography
Although not always necessary to diagnose cardiac tamponade, echocardiography is the most useful tool for diagnosing the underlying pericardial disease and may be the only way to detect small volumes of pericardial effusion.21 A thorough echocardiogram allows rapid confirmation of the presence of pericardial effusion (Figure 5); identify intrapericardial masses (Figure 6), including blood clots; observe evidence of left atrial rupture; assess the thickness of the pericardium; evaluate cardiac tamponade; and confirm the presence or absence of pleural effusion. The presence of bowel loops, stomach, or other abdominal organs in the pericardial sac confirms a diagnosis of peritoneopericardial diaphragmatic hernia. Abdominal ultrasonography of older dogs with pericardial effusion is useful in identifying splenic or liver neoplasia. Hepatic vein distention and ascites support the presence of increased systemic venous pressure, though this finding is not restricted to patients with cardiac tamponade.13
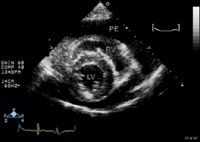
5. A short-axis echocardiogram obtained from the right parasternal window in a dog. Note the pericardial effusion (anechoic area) surrounding the heart (RV=right ventricle; LV=left ventricle; PE=pericardial effusion).
Pericardial fluid analysis
Pericardiocentesis is vital for therapeutic purposes if tamponade is present, and it also can be useful to collect samples for diagnostic testing. Collect samples in EDTA tubes and plain tubes for submission to a laboratory for cytologic examination and bacterial culture and antimicrobial sensitivity testing if indicated. Diagnosis of a neoplastic process is difficult because reactive mesothelial cells are often present in effusions even when the underlying process is benign. However, cytologic examination is occasionally helpful, particularly if an inflammatory process is likely. Fluid pH was once reported to help distinguish between neoplastic and idiopathic effusions, but a recent study has shown that the overlap between the two groups is too great to be of diagnostic utility.22
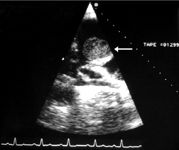
6. A right parasternal echocardiogram obtained at the heart base in a dog. Note the hypoechoic mass (arrow) on the right atrial appendage that is the presumptive cause of the effusion. The mass was a hemangiosarcoma.
TREATMENT
Treatment of pericardial disease is aimed at correcting the underlying disorder or attempting to minimize its impact on cardiac function. When cardiac tamponade is present, emergent removal of pericardial fluid is indicated. Reduction in pericardial pressure after fluid removal leads to an immediate increase in cardiac output, a decrease in heart rate, and a marked improvement in the patient's clinical status. Large volume ascites that develops secondary to cardiac tamponade can be removed if the patient is experiencing ventilatory compromise or discomfort.23 However, in most cases, once cardiac tamponade is relieved, ascites will resolve rapidly because of diuresis. Diuretic medications are also not necessary. In general, long-term management and therapy are typically focused on the subset of patients with recurrent pericardial effusion. If initial therapy is ineffective or if the effusion becomes recurrent, more definitive procedures, such as pericardiectomy, are recommended.
Pericardiocentesis
For a discussion on pericardiocentesis, including a step-by-step description of the procedure, see "How to perform a pericardiocentesis".
Pericardiectomy
A complete discussion of pericardiectomy procedures is beyond the scope of this article. Although historically performed via thoracotomy, many of these procedures are now performed via thoracoscopy and involve either making a window in the pericardium or removing most of the pericardium (subtotal pericardiectomy).1 Other minimally invasive procedures (e.g. balloon pericardial windows) have proven successful.1 For chronic diseases such as idiopathic hemorrhagic pericardial effusion, any fluid that would have accumulated in the pericardial sac is simply reabsorbed via the mediastinal vasculature and lymphatics.
PROGNOSIS
The prognosis for a patient with pericardial disease depends on the underlying etiology, varying from excellent to grave. See the discussion under individual etiologies for more detail.
CONCLUSION
The successful management of pericardial disease in small animals depends on rapidly diagnosing and managing cardiac tamponade, if present. Even a small volume of effusion can significantly impact cardiac output when it leads to cardiac tamponade.
Mark D. Olcott, DVM
Animal Emergency & Critical Care
165 Ft. Evans Road NE
Leesburg, VA 20176
Meg M. Sleeper, VMD, DACVIM (cardiology)
Section of Cardiology
Department of Clinical Studies
Veterinary Hospital of the University of Pennsylvania
Philadelphia, PA 19104
REFERENCES
1. Nelson OL, Ware WA. Pericardial effusion. In: Bonagura JD, Twedt DC, eds. Current veterinary therapy XIV. St. Louis, Mo: Elsevier, 2009;825-831.
2. Sisson D, Thomas WP. Pericardial disease and cardiac tumors. In: Fox PR, Sisson D, Moise NS, eds. Textbook of canine and feline cardiology. 2nd ed. Philadelphia, Pa: Saunders, 1999;679-699.
3. Buchanan JW. Causes and prevalence of cardiovascular disease. In: Kirk RW, Bonagura JD, eds. Kirk's current veterinary therapy XI: small animal practice. Philadelphia, Pa: WB Saunders, 1992;647-655.
4. Ware WA, Hopper DL. Cardiac tumors in dogs: 1982-1995. J Vet Intern Med 1999;13(2):95-103.
5. Laste NJ. Pericardial diseases. In: Silverstein DC, Hopper K, eds. Critical care medicine. St. Louis, Mo: Elsevier, 2009;184-188.
6. Vicari ED, Brown DC, Holt DE, et al. Survival times of and prognostic indicators for dogs with heart base masses: 25 cases (1986-1999). J Am Vet Med Assoc 2001;219(4):485-487.
7. Stafford Johnson M, Martin M, Binns S, et al. A retrospective study of clinical findings, treatment and outcome in 143 dogs with pericardial effusion. J Small Anim Pract 2004;45(11):546-552.
8. Berg RJ, Wingfield WE, Hoopes PJ. Idiopathic hemorrhagic pericardial effusion in eight dogs. J Am Vet Med Assoc 1984;185(9):988-992.
9. Hall DJ, Shofer F, Meier CK, et al. Pericardial effusion in cats: a retrospective study of clinical findings and outcome in 146 cats. J Vet Intern Med 2007;21(5):1002-1007.
10. Davidson BJ, Paling AC, Lahmers SL, et al. Disease association and clinical assessment of feline pericardial effusion. J Am Anim Hosp Assoc 2008;44(1):5-9.
11. Reimer SB, Kyles AE, Filipowicz DE, et al. Long-term outcome of cats treated conservatively or surgically for peritoneopericardial diaphragmatic hernia: 66 cases (1987-2002). J Am Vet Med Assoc 2004;224(5):728-732.
12. Reineke EL, Burkett DE, Drobatz KJ. Left atrial rupture in dogs: 14 cases (1990-2005). J Vet Emerg Crit Care 2008;18(2):158-164.
13. Sisson D, Kittleson MD. Management of heart failure: principles of treatment, therapeutic strategies, and pharmacology. In: Fox PR, Sisson D, Moise NS, eds. Textbook of canine and feline cardiology. 2nd ed. Philadelphia, Pa.: Saunders, 1999;216-250.
14. Madewell BR, Norrdin RW. Renal failure associated with pericardial effusion in a dog. J Am Vet Med Assoc 1975;167(12):1091-1093.
15. Kienle, RD. Pericardial disease and cardiac neoplasia—Pathophysiology. In: Kittleson MD, Kienle RD, eds. Small animal cardiovascular medicine. 2nd ed. St. Louis, Mo.: Elsevier, 2007.
16. Rush JE, Keene BW, Fox PR. Pericardial disease in the cat: a retrospective evaluation of 66 cases. J Am Anim Hosp Assoc 1990;26:39-46.
17. Kittleson MD. Signalment, history, and physical examination—Physical examination—Part I. In: Kittleson MD, Kienle RD, eds. Small animal cardiovascular medicine. 2nd ed. St. Louis, Mo.: Elsevier, 2007.
18. Bonagura JD. Pericardial diseases and pericardiocentesis in the dog, in Proceedings. Br Small Anim Vet Congress 2007.
19. Tobias AH, McNiel EA. Pericardial disorders and cardiac tumors. In: Tilley L, Smith F, Oyama M, et al, eds. Manual of canine and feline cardiology. 4th ed. St. Louis, Mo.: Elsevier, 2008;200-214.
20. Sacks E, Widman LE: Nonlinear heart model predicts range of heart rates for 2:1 swinging in pericardial effusion. Am J Physiol 1993;264(P5 Pt 2):H1716-H1722.
21. Abbott JA. Pericardial disease—Diagnosis and therapy, in Proceedings. Am Coll Vet Intern Med Forum 2006;217.
22. Fine DM, Tobias AH, Jacob KA. Use of pericardial pH to distinguish between idiopathic and neoplastic effusions. J Vet Intern Med 2003;17(4):525-529.
23. Kittleson MD. Management of heart failure—ancillary therapy. In: Kittleson MD, Kienle RD, eds. Small animal cardiovascular medicine. 2nd ed. St. Louis, Mo.: Elsevier, 2007. ã
Podcast CE: Canine cardiology: the practical guide to the mitral valve patient
July 19th 2023Learn about the prevalence of myxomatous mitral valve disease, guidelines for staging heart disease, proactive diagnostic workup, the importance of spironolactone and aldosterone blocking, and the benefits of combination therapy for improved outcomes in canine patients
Listen