Three-minute peripheral blood film evaluation: The leukon
In this article, we again use a question-based format to guide you in evaluating the leukon by assessing white blood cell numbers and morphology.
In the previous article, we discussed how to examine the erythron and thrombon components of peripheral blood films. In this article, we again use a question-based format to guide you in evaluating the leukon by assessing white blood cell (WBC) numbers and morphology. All five WBC cell types are assessed. Table 1 lists the general patterns of WBC response under a variety of circumstances.
Table 1 Common Leukocyte Patterns in Dogs and Cats
Is the total WBC count elevated, normal, or decreased?
Experience is required to accurately estimate cell counts directly from blood films. Subjective analysis of total WBC numbers may be performed by counting three to five 20X objective fields; 10 to 20 WBCs/20X field is considered normal in dogs and cats. Another method involves counting several 100X oil-immersion monolayer fields and multiplying the average number of WBCs/100X oil-immersion field by 2,000 to obtain a final estimated total WBC count.1
Is a left shift present?
A left shift may be the only indicator of active inflammation in veterinary patients because total WBC and neutrophil counts are frequently within the reference range. Left shifts are characterized by increased numbers of immature neutrophils (e.g. band cells, metamyelocytes) in circulation. A left shift is a hallmark of inflammation, so accurately identifying band cells is extremely valuable. No hematology analyzer (in-house or reference laboratory instrumentation) has been documented to accurately identify band neutrophils; consequently, they must be identified microscopically. On blood films, the nucleus of a band neutrophil typically has parallel sides (Figure 1), whereas the nucleus of a mature neutrophil is distinctly segmented. One useful approach to differentiate band neutrophils is to estimate the degree of nuclear indentation. First, identify the narrowest and widest portions of the nucleus. If the narrowest portion is less than one-third of the widest portion, the cell is classified as a band cell.1
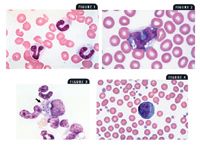
Figure 1. Canine band neutrophils (modified Wright's stain; 100X). Figure 2. A canine monocyte (modified Wright's stain 100X). Figure 3. A buffy coat smear from a dog showing a macrophage (arrow) phagocytizing Histoplasma species (modified Wright's stain 100X). Figure 4. A reactive lymphocyte in a dog (modified Wright's stain 100X).
Is there a monocytosis?
The monocyte-macrophage continuum represents the second major branch of the circulating phagocyte system (neutrophils are the first). Monocytes (
Figure 2,
), unlike granulocytes (neutrophils, eosinophils, basophils), are released into the peripheral blood as immature cells and then differentiate into phagocytic macrophages (
Figure 3
), epithelioid macrophages, or multinucleated giant cells.
Monocytosis can be another indicator of inflammation. It may be seen in both acute and chronic conditions but may also be a component of stress leukograms. Conditions frequently associated with monocytosis include systemic fungal diseases (histoplasmosis, blastomycosis, cryptococcosis, coccidioidomycosis, aspergillosis), immune-mediated hemolytic anemia, bacterial endocarditis, certain neoplastic diseases (particularly when tissue necrosis is noted), and certain pyogranulomatous diseases (e.g. feline infectious peritonitis, toxoplasmosis, foreign body reactions).2 The best interpretation of monocytosis in the absence of a stress leukogram is tissue demand for macrophages.
Is a persistent eosinophilia present?
Persistent eosinophilia indicates a systemic hypersensitivity reaction and can be another indicator of inflammation. Conditions associated with persistent eosinophilia include heartworm disease in dogs and cats, feline asthma, canine atopic syndromes, feline eosinophilic granuloma complex (linear plaque form), hypereosinophilic syndrome, mast cell leukemia, and flea allergy dermatitis.3 Parasitic infections confined to the bowel, such as whipworm infections or ascarid and hookworm infections in adult nonpregnant dogs and cats, do not cause persistent peripheral eosinophilia because the parasites do not have a systemic phase.4
Are reactive or atypicallymphocytes present?
The presence of reactive lymphocytes (Figure 4) simply suggests systemic antigenic stimulation. This stimulation could be in response to a recent vaccination, an infectious disease, or another process stimulating the immune system. The most commonly identified morphologic change associated with lymphocyte reactivity is increased amounts of basophilic cytoplasm.
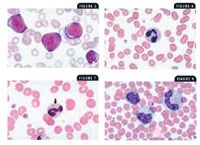
Figure 5. Atypical lymphocytes in a dog (modified Wright's stain; 100X). Figure 6. Mild neutrophil toxicity in the form of cytoplasmic basophilia in a cat (modified Wright's stain; 100X). Figure 7. Moderate neutrophil toxicity in the form of Döhle bodies (arrow) in a cat (modified Wright's stain; 100X). Figure 8. Marked neutrophil toxicity in a dog. Note the cellular giantism and basophilic, foamy, vacuolated cytoplasm (modified Wright's stain; 100X).
Atypical lymphocytes (Figure 5) are abnormal lymphocytes characterized by increased size with indented or cleft nuclei and large azurophilic cytoplasmic granules. These cells are not disease-specific and may be present with infectious and neoplastic conditions. Atypical lymphocytes require additional investigation by a clinical pathologist. Bone marrow examination and detailed cytologic and possible histologic evaluation of peripheral and internal lymphoid tissues may also be recommended.
Are toxic neutrophils present?
Toxic neutrophils are a result of an accelerated rate of neutrophil production in response to inflammatory signals received by the bone marrow. Toxic neutrophil changes include retention of cytoplasmic features of immaturity and include foamy basophilic cytoplasm (Figure 6) and small basophilic precipitates known as Döhle bodies (Figure 7). Döhle bodies are often present in low numbers in normal cats, so, by themselves, they are a relatively equivocal finding; but Döhle bodies indicate serious toxicity in dogs.5 Other toxic changes include bizarre nuclear shapes and cellular giantism (Figure 8).
Systemic toxemia is often associated with bacterial endotoxins, but noninfectious causes also occur. Infectious diseases commonly accompanied by severe neutrophil toxicity include feline pyothorax, pyometra, and severe canine prostatitis. Noninfectious causes associated with toxemia include immune-mediated hemolytic anemia, acute pancreatitis, tissue necrosis, zinc and lead toxicosis, and cytotoxic drug therapy.6
Conclusion
Evaluating the five different WBC types is critical when you develop a differential diagnosis list. Increases or decreases in neutrophils, eosinophils, basophils, lymphocytes, and monocytes should alert you to investigate certain conditions. For example, neutrophilic left shifts, persistent eosinophilia, and monocytosis are indicators of inflammation: Left shifts (increased numbers of immature, or band, neutrophils in circulation) indicate increased turnover and tissue use of neutrophils. Persistent peripheral eosinophilia indicates a systemic allergic or hypersensitivity reaction. And monocytosis is seen in peripheral blood when a demand for phagocytosis is present.
Fred L. Metzger Jr., DVM, DABVP (canine and feline practice)
Metzger Animal Hospital
1044 Benner Pike
State College, PA 16801
Alan Rebar, DVM, PhD, DACVP
Department of Veterinary Pathobiology
School of Veterinary Medicine
Purdue University
West Lafayette, IN 47907
ACKNOWLEDGMENT
The authors gratefully acknowledge the technical assistance and images provided by Dennis DeNicola, DVM, PhD, DACVP.
REFERENCES
1. Rebar, A.; Metzger, F.: The Veterinary CE Advisor: Interpreting Hemograms in Cats and Dogs. Vet. Med. (suppl.) 96 (12):1-12; 2001.
2. Duncan, J. et al.: Erythrocytes, leukocytes, hemostasis. Veterinary Laboratory Medicine, 3rd Ed. Iowa State University Press, Ames, 1994; pp 75-93.
3. Willard, M. et al.: Leukocyte disorders. Textbook of Small Animal Clinical Diagnosis by Laboratory Methods, 3rd Ed. W.B. Saunders, Philadelphia, Pa., 1999; pp 53-79.
4. Rebar, A.H. et al.: Laboratory methods in hematology. A Guide to Hematology in Dogs and Cats. Teton New Media, Jackson, Wyo., 2002; pp 10-28.
5. Willard, M. et al.: The complete blood count and bone marrow examination. Textbook of Small Animal Clinical Diagnosis by Laboratory Methods, 3rd Ed. W.B. Saunders, Philadelphia, Pa., 1999; pp 11-30.
6. Duncan, J. et al.: Erythrocytes, leukocytes, hemostasis. Veterinary Laboratory Medicine, 3rd Ed. Iowa State University Press, Ames, 1994; pp 75-93.