A guide to regional analgesia of the head in equine patients
With the right tools and technique, you can avoid general anesthesia and still provide adequate analgesia during surgery. Here's your guide to several nerve blocks in your veterinary equine patients.
Appropriate regional analgesia is a cornerstone for successful standing surgery in horses. When combined with an appropriate sedative protocol, many surgical procedures can now be performed standing, avoiding the cost and risks associated with general anesthesia. Performing standing surgical procedures of the head provides improved visualization and hemostasis, reduces morbidity, and eliminates the need for specialized equipment and facilities.
Read on to discover how to perform regional blocks on the equine head, where to expect analgesia, the potential complications that you may encounter, and examples of surgical procedures and diagnostic techniques that use these blocks.
Patient prep
A sterile prep is recommended, particularly for the maxillary and inferior alveolar nerve blocks because of the depth of the nerve block and limited drainage these sites provide should an infection set in within the region that is injected. Special care is warranted to keep disinfectant from contacting the cornea.
Maxillary nerve block
The maxillary nerve block is a mainstay for performing dental extractions in the upper arcades. It blocks the upper incisors, canines, premolars and molars and is an essential block for standing sinus surgery in horses. I've also used it for standing repair of incisive and rostral maxillary fractures with wire fixation. Other uses include localization of neuropathy for horses that are head shakers and to aid in the repair of extensive lacerations involving the upper lips or face dorsal to the facial crest and rostral to the eye.
Multiple techniques are described. Many describe placing an 18- to 22-ga, 3.5-in (9-cm) spinal needle toward the maxillary nerve as it enters the pterygopalatine fossa at the maxillary foramen. One technique places the spinal needle ventral to the zygomatic process at the level of the caudal orbit, advancing rostromedially until hitting bone (Figure 1A).1

Figure 1A. Performing a maxillary nerve block by placing a spinal needle below the zygomatic process to block the maxillary nerve. (All photos courtesy of Dr. Nick Carlson)The other technique places the needle dorsal to the union of the zygomatic bone and zygomatic process of the frontal bone angled ventrally 20 degrees from the horizontal plane until it contacts bone (Figure 1B).1

Figure 1B. An alternative method to block the maxillary nerve by placing the needle above the zygomatic bone.In both cases, 10 to 15 ml of local anesthetic is deposited, and analgesia should occur in 15 to 20 minutes. The use of ultrasound has been advocated for this block to improve accuracy of needle placement.2 Both techniques pose the risk of vessel laceration and exophthalmos, so I do not advocate them.
My preferred method is placing a 1.5-in (3.8-cm), 20- to 22-ga needle ventral to the zygomatic process at the level of the caudal aspect of the orbit and burying the needle to allow it to pass through the masseter muscle and into the extraperiorbital fat (Figure 2).3

Figure 2. A: A safer approach to blocking the maxillary nerve using a 1.5-in, 20-ga needle. Needle placement and trajectory mimics the traditional maxillary nerve block with a spinal needle demonstrated in Figure 1A. Inset--B: This places the needle in the periorbital fat away from large vasculature.Inject a larger volume (20 to 30 ml) of local anesthetic. You can ensure proper placement by observing the filling of the supraorbital pouch. Here the needle is placed away from large vessels, resulting in fewer complications.
The most frequently encountered complication with a maxillary nerve block is development of a hematoma or an abscess at the injection site, leading to exophthalmos that may require a temporary tarsorrhaphy or frequent application of eye ointment by the owner until resolved. Other complications include temporary blindness, pupil dilation or orbital protrusion from loss of function of the optic nerve and oculomotor function.1 Using a shorter needle and placing the block in the supraorbital fat pad minimizes most of these complications.
Infraorbital nerve block
The infraorbital nerve is an extension of the maxillary nerve as it travels through the infraorbital canal. The traditionally described infraorbital block will only block the incisors and premolars but will not fully anesthetize the molars or paranasal sinuses. Recently, it has been shown that a larger volume (10 ml versus 3 to 5 ml) should travel retrograde through the canal to fully anesthetize these structures, similar to a maxillary nerve block.4
To locate the left foramen, place the thumb of your left hand on the rostral most aspect of the facial crest and the middle finger of the same hand in the nasomaxillary notch. The index finger of the left hand should then fall over the foramen (Figure 3).

Figure 3. An example of hand placement to identify the infraorbital foramen to perform an infraorbital nerve block. The thumb is placed on the rostral facial crest and the middle finger in the nasal notch. This will place the index figure near the foramen, which is identified as a depression under the skin.In some horses, the ventral edge of the levator nasolabialis muscle requires elevation to expose the palpable notch under the skin.1 Insert a 20- to 22-ga, 1.5-in (7.63-cm) needle through the skin 1 to 2 cm rostral to the palpable notch, and, if possible, fully bury the needle into the canal. Inject a volume of 5 to 10 ml of local anesthetic. Confirmation of proper needle placement is moderate pressure during the injection and lack of development of a subcutaneous bleb during injection.
Caution is advised during block placement as violent objection by the horse can occur despite heavy sedation and restraint if the needle contacts the nerve. A small bleb of local anesthesia can be placed over the entrance of the foramen to improve the horse's tolerance, but this makes palpation of the foramen difficult.
Few complications with use of this block are described. Theoretically, the nerve could be lacerated by the needle as it is placed into the foramen leading to neuroma formation or infection in the canal and subsequent neuritis.
If you are extracting maxillary incisors, combining an infraorbital nerve block with 5 ml of local anesthetic at the incisive canal on the midline of the rostral incisive bone where the lip and gingival tissue meet will enhance the infraorbital block.
Inferior alveolar nerve block (mandibular nerve block)
The inferior alveolar nerve innervates the lower arcade, mandible and lower lips. Blocking the inferior alveolar nerve is primary used to extract premolars and molars in the lower arcade. It can also be used for débridement of deep periodontal pocketing associated with diastemas, débridement of mandibular drainage tracks, and wire fixation of rostrally located mandibular fractures in standing horses.
Two techniques exist for blocking the inferior alveolar nerve. The traditional blind technique is performed by guiding a long (8- to 10-in) 18- to 20-ga spinal needle on the medial mandible to the mandibular foramen and depositing 20 to 30 ml of local anesthetic. The mandibular foramen is estimated by the intersection of a vertical line drawn from the caudal aspect of the orbit and a horizontal line parallel to the occlusal surface of the lower cheek teeth (Figure 4).1

Figure 4. A: The blind technique for the inferior alveolar nerve block. The needle is guided to a target created by intersecting a vertical line drawn behind the caudal rim of the orbit and a horizontal line following the trajectory of the lower arcade's occlusal surface (red lines). The needle (white line) is advanced on the inside of the mandible with an effort made to scrape against the periosteum to ensure the needle does not migrate too axially. Inset--B. An example of needle placement adjacent to the inferior alveolar nerve.Intermittent contact with the periosteum during needle advancement ensures the needle does not deviate axially away from the mandible that could place the needle in the tongue base, oral cavity or soft palate.
More recently, an intraoral approach was reported to anesthetize the inferior alveolar nerve. To perform this nerve block, 12-in-long locking clamp pliers are used to secure a 20-ga, 1.5-in (3.8-cm) needle bent 20 to 30 degrees attached to an extension set. The target for injection is the mucosa just caudal and above the table surface of the third mandibular molar and lateral to the palate.5 Before performing the block, a thorough lavage of the mouth is performed, followed by packing a gauze soaked in local anesthetic into the injection site for two to three minutes. The site is then prepped by repeat application of chlorhexidine-soaked gauze for a contact time of five minutes. The needle is placed and buried at the injection site, trying to stay close to the medial aspect of the mandible (Figure 5).
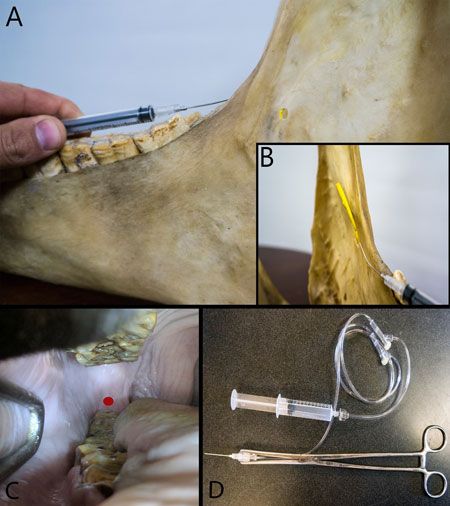
Figure 5. A--Needle placement for the intraoral inferior alveolar nerve block. The needle is placed on the medial aspect of the mandible in the soft tissue caudal to the last molar at the level of the molar's occlusal surface. B--An image showing the needle's placement over the nerve's insertion into the mandible. C--An intraoral image with the red dot depicting the site for needle placement. D--Tools used to perform the block on a horse: 12-in-long grasping forceps; 20-ga, 1.5-in needle; extension set and 12-ml syringe.About 5 to 7 ml of local anesthetic is injected. This is now the method I prefer to perform this block.
Complications are more common when using the blind technique and include block failure from improper placement, hematoma or abscess formation, and horse-inflicted trauma to the tongue from inadvertent blocking of the lingual nerve. Some advocate using shorter-acting anesthetics, withholding feed or using a mouth gag until the anesthetic has fully worn off to avoid potential trauma to the tongue by inadvertently blocking of the lingual nerve.
Mental nerve block
Like the infraorbital nerve, the mental nerve is a continuation of its parent nerve (inferior alveolar nerve). It exits the mandible through the mental foramen. Blocking this nerve will desensitize the rostral mandible, canines, incisors and lower lip. To locate the mental foramen, feel for the depression on the lateral mandible rostral to the first cheek tooth. On some horses, the depressor labii inferioris muscle must be retracted dorsally to palpate the foramen.1 A 1.5-in (3.8-cm) needle with a 15- to 20-degree bend is placed through the skin rostral to the foramen and directed caudally to bury the needle, if possible; then deposit 3 to 5 ml of local anesthetic (Figure 6).

Figure 6. The mental nerve block is performed by identifying the mental foramen rostral to the first lower premolar.
A moderate pressure during injection of the local anesthetic and lack of blebbing at the injection site confirms proper needle placement. This block is exceedingly difficult to place because of the foramen's location in proximity to the lower lips, inhibiting a straight trajectory of the needle path from the skin to the foramen. This is exacerbated by the violent objection some horses exhibit if the needle contacts the nerve. I rarely perform this block because of its difficult location and objection by the horse and will instead opt to use the inferior alveolar nerve block.
Auriculopalpebral nerve block
The auriculopalpebral nerve is a branch of the facial nerve and innervates the motor nerves of the upper eyelid. To perform the block, insert a 25-ga, 5/8-in needle containing 3 to 5 ml of local anesthetic at the dorsal edge of the most dorsal point of the zygomatic arch.6 This block is only motor and produces no loss of sensation. It's commonly used for ophthalmic exams but is also beneficial for many ophthalmic surgeries to reduce blepharospasm.
Eyelid desensitization
The following blocks are commonly used during enucleation and can also aid in eyelid repair surgery. The portion of the lid blocked by each nerve is shown in Figure 7A.
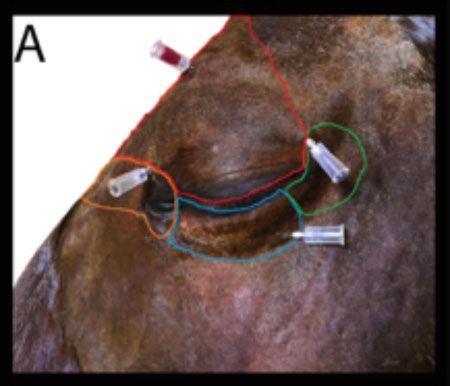
Figure 7A. The locations for blocking eyelid sensation: supraorbital/frontal nerve (red), lacrimal nerve (green), zygomatic nerve (blue) and intratrochlear nerve (orange).Supraorbital nerve block
The frontal nerve innervates the medial two-thirds of the upper lid. The nerve can be blocked as it exits the supraorbital canal. The supraorbital canal is a palpable depression found by placing the thumb on the dorsal rim of the orbit and the middle finger in the supraorbital fossa. The index finger placed between these two fingers should fall into the supraorbital canal. Bury a 25-ga 5/8-in needle and deposit 3 to 4 ml of local anesthetic.6
Lacrimal nerve
The lacrimal nerve is blocked by placing a 25-ga, 5/8-in needle in the lacrimal notch, which is palpated on the dorsolateral rim of the orbit or by using a line block on the lateral third of the dorsal orbital rim with 1 to 3 ml of local anesthetic.6 This will anesthetize the lateral canthus.
Zygomatic nerve
The zygomatic nerve is blocked via a line block along the ventrolateral orbital rim with 2 to 3 ml of local anesthetic.6 This will anesthetize the lower eyelid.
Infratrochlear nerve
The infratrochlear nerve is blocked as it runs through the trochlear notch on the medial aspect of the dorsal orbital rim with 1 to 2 ml of local anesthetic with a 25-ga, 5/8-in needle.6 This will anesthetize the medial canthus including the third eyelid.
Retrobulbar nerve block
This nerve block will temporarily block the optic, oculomotor, abducens and trochlear nerves and the maxillary and ophthalmic branches of the trigeminal nerve. It's an important block to desensitize the ocular surface for standing corneal surgery and the globe for enucleation. The block is performed aseptically with a 20- to 22-ga, 3.5-in spinal needle placed through the skin perpendicular to the skull in the orbital fossa just caudal to the caudal aspect of the dorsal orbital rim (Figure 7B).

Figure 7B. The location of the retrobulbar nerve block using a 3-in spinal needle placed against the rim of the zygomatic bone in the supraorbital pouch and advanced until a "pop" is felt as the needle penetrates through the fascia of the optic cone.The needle is advanced caudal to the globe until it falls into the retrobulbar cone.6 A slight dorsal movement of the eye is observed as the needle passes through the fascia of the dorsal retrobulbar cone into the retrobulbar space. When the needle passes into the cone, a sudden "pop" should be felt and the eye should fall back into its normal position. Place a volume of 10 to 12 ml of local anesthetic into the space. Slight exophthalmos occurs and the block should take effect in five to 10 minutes. Ocular sensation, corneal reflex and vision are all blocked, so if the goal of surgery is to preserve the eye, frequent lubrication or a temporary tarsorrhaphy is required for two to four hours after the procedure.
Complications include reaction to the anesthetic causing significant retrobulbar swelling, corneal ulcer from exposure keratitis, and cellulitis or abscess formation. Rarely retrobulbar hemorrhage, optic neuritis and elicitation of the oculocardiac reflex can occur.
The four-point block can also be used to block the retrobulbar space, but due to the larger volume used this block puts greater pressure on the globe and can lead to severe chemosis, complicating surgeries of the globe and orbit. Thus, it has no advantages over the single injection technique.
References
1. Doherty T, Schumacher J. Dental restraint and anesthesia. In: Easley J, Dixon PM, Schumacher J, eds. Equine dentistry. 3rd ed. Maryland Heights, Michigan: Elsevier, 2011;241-244.
2. O'Neill HD, Garcia-Pereira FL, Mohankumar PS. Ultrasound-guided injection of maxillary nerve in the horse. Equine Vet J 2014:46:180-184.
3. Staszyk C, Bienert A, Baumer W, et al. Simulation of local anaesthetic nerve block of the infraorbital nerve within the pterygopalatine fossa: anatomical landmarks defined by computed tomography. Res Vet Sci 2008;85:399-406.
4. Nannarone S, Bini G, Vuerich M, et al. Retrograde maxillary nerve perineural injection: A tomographic and anatomic evaluation of infraorbital canal and evaluation of needle type and size in equine cadavers. Vet J 2016;217:33-39.
5. Henry T, Pusterla N, Guedes AG, et al. Evaluation and clinical use of an intraoral inferior alveolar nerve block in the horse. Equine Vet J 2014;46:706-710.
6. Gilger BC, Stoppini R. Equine ocular examination: routine and advanced diagnostic techniques. In: Gilger BC, ed. Equine ophthalmology. 2nd ed. Maryland Heights, Michigan: Elsevier, 2016;11-13.
Dr. Nick Carlson is a board-certified large animal surgeon at Steinbeck Country Equine Hospital in Salinas, California. He has a specific interest in equine dentistry and upper airway disorders in horses. In his spare time, he enjoys exploring his home state of California with his wife and their two young boys.