Pediatric dentistry: An overview of common problems you'll see in practice
This article focuses on the more common oral and dental problems diagnosed during the pediatric dental period. Some of these problems are quite similar to problems seen in adult patients, while others are confined to younger patients.
Pediatric dentistry is generally defined as the dental care of animals from birth to about 1 year of age. At 1 year of age, the permanent dentition has matured and adult dental issues begin. This article focuses on the more common oral and dental problems diagnosed during the pediatric dental period. Some of these problems are quite similar to problems seen in adult patients, while others are confined to younger patients.
PERSISTENT DECIDUOUS DENTITION
The most common pediatric dentistry problem is persistent deciduous teeth (previously known as retained deciduous teeth).1 A deciduous tooth is considered persistent as soon as the permanent tooth begins to erupt into the mouth.
Cause and predisposition
The most frequent cause of deciduous tooth persistence is an incorrect eruption path of the permanent tooth.2 When the permanent tooth erupts along its natural path, it places pressure on the apex of the deciduous tooth, resulting in deciduous root end resorption.3 This resorption progresses until the deciduous tooth exfoliates and the permanent tooth assumes its normal position in the mouth. When the permanent tooth follows an incorrect path, there will be no impetus for deciduous root resorption, resulting in the deciduous tooth's retention and the permanent tooth's eruption alongside.
Because of the pattern of occurrence, especially within certain breeds and head types, persistent deciduous teeth are generally viewed as a genetic problem.2 This view counters the mistaken belief that the persistent deciduous tooth caused the permanent tooth to erupt in an unnatural position.
Other causes of persistent deciduous dentition are rare but include primary impaction or ankylosis of the deciduous tooth. These conditions will not allow for normal exfoliation and result in either impaction or improper eruption of the permanent tooth.2
Persistent deciduous dentition occurs most often in toy- and small-breed dogs but can be seen in any breed as well as in cats. The most common deciduous teeth to become persistent are the cuspids (previously known as canines), followed by the incisors and then the premolars.2
Diagnosis
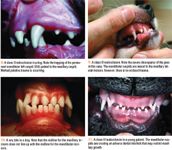
An oral examination will reveal extra teeth in the arcades (Figure 1). This extra dentition is typically bilateral and results in crowding. In addition, the permanent dentition will be in an abnormal position, which may cause dental, gingival, or palatine trauma. Orthodontic changes can occur within two weeks of the first sign of eruption of the permanent dentition.2

Because the deciduous tooth and the permanent tooth share the same gingival attachment, the permanent tooth is not allowed to develop a normal gingival attachment, resulting in susceptibility to periodontal disease.2 Patients that tend to retain teeth (e.g. toy- and small-breed dogs) are also prone to developing periodontal disease in general.
In animals with persistent deciduous teeth, the permanent tooth does not need to be completely erupted for orthodontic and periodontal problems to occur. In fact, the problems start as soon as the permanent tooth begins to erupt.
All persistent deciduous teeth must be extracted as early as possible to lessen the untoward effects.2,4 The age at eruption of permanent incisors, cuspids, and premolars is between 3 and 6 months,4 which approximately parallels the timing of the last vaccination in most puppy or kitten immunization series. Therefore, it is strongly recommended that an oral evaluation accompany this visit. In addition, instruct owners to examine their pets' mouths on a regular basis to help ensure the prompt detection and removal of these teeth. Because damage begins shortly after eruption of the permanent tooth, it is not recommended to wait to perform deciduous tooth extraction along with an ovariohysterectomy or orchiectomy.
Obtain a diagnostic dental radiograph to help differentiate the deciduous teeth from permanent dentition in questionable cases. Radiographs will also confirm the integrity of the root structure of the deciduous teeth (Figure 2).
Treatment
Deciduous tooth extraction can be difficult because of the considerable length and thin walls of deciduous teeth (Figure 3). Resorption and ankylosis of the persistent deciduous teeth can further complicate extraction. Consequently, deciduous tooth root fracture is common during extraction attempts. When fracture occurs, make every effort to remove the root apex as it may become infected or act as a foreign body, leading to marked inflammation.4 Clinical signs are rarely associated with deciduous tooth root fracture, but the patient will experience severe pain from the exposed nerve, which will then become a source of chronic bacterial infection following tooth necrosis. Since a retained root tip is sufficient to deflect the permanent tooth from its normal eruptive path, complete removal is even more critical in cases of interceptive orthodontics (see "Dental terms and definitions").4

Dental terms and definitions
Deciduous tooth extractions should be done carefully to avoid damaging the permanent tooth.2 Some veterinary dentists surgically extract these teeth to decrease the possibility of causing iatrogenic damage. Obtain a postoperative dental radiograph to confirm complete extraction of the deciduous tooth as well as to document the continued presence and proper condition of the permanent tooth.
FRACTURED DECIDUOUS TEETH
Any deciduous tooth can fracture, but fracture of the cuspids is by far the most common. The fracture is almost always traumatic in origin (e.g. caused by being hit by a ball, bat, or car; falling; or abnormal chewing behavior). Deciduous teeth are longer and have thinner walls than their permanent counterparts, so they are more prone to fracture.5 In addition, the relatively larger size of the pulp chamber ensures that almost any deciduous tooth fracture will result in pulp exposure.4
Diagnosis
On oral examination, a fractured deciduous tooth will be shorter than the contralateral tooth and the pulp will be evident. If the fracture is fresh, it will be pink and may be bleeding (Figure 4). Because of the large size of the endodontic system, pulp infection and abscessation occur quickly.5 If abscessation has occurred, the pulp will be dark-brown or black, and a draining tract may be present at or near the root apex (Figure 5). These abscesses drain directly onto the crown of the developing permanent tooth, which may result in damage such as enamel hypocalcification.5,6
Evaluate dental radiographs of the fractured tooth to ensure that it is a deciduous tooth and to determine deciduous root presence and integrity, as well as the proximity of the permanent tooth.5 Commonly, the roots will be undergoing resorption, making extraction challenging.
Treatment
Extracting the fractured tooth is the treatment of choice. Extraction will alleviate the pain and potential infection from the exposed dental pulp. If deciduous tooth extraction will result in the loss of a valued dental interlock, vital pulp therapy or root canal therapy may be performed.4 An additional benefit of endodontic therapy is the avoidance of scar formation, which could result in an impacted permanent tooth.

MALOCCLUSIONS
Several types of malocclusions exist, which are divided into four classes.
- Class 0 occlusions are normal. In most breeds, a class 0 occlusion is present when the maxillary incisors overlap the mandibular incisors, and the incisal edges of the mandibular incisors rest on or near the cingulum of the maxillary incisors (scissor bite).7 In addition, the mandibular cuspids should interdigitate between the maxillary cuspids and maxillary lateral incisors (Figure 6). However, brachycephalic breeds are considered class 0 with a mandible that is longer than the maxilla. This is also referred to as a class 0, type III occlusion.8
- A class I malocclusion occurs when there is a normal jaw length but one or more teeth are out of alignment. Examples of class I malocclusions include mesioclusion of a maxillary cuspid (lance effect) (Figure 7) and linguoversion of a mandibular cuspid (base narrow).
- A class II malocclusion, or overshot, exists when the maxilla is longer than the mandible (Figure 8).
- A class III malocclusion, or undershot, occurs when the mandible is longer than the maxilla (Figure 9). This occlusion is considered class 0, or normal, in brachycephalic breeds.
- A class IV malocclusion occurs when one mandible is longer and the other is shorter than the maxilla.7 Keep in mind that a wry bite, which is a jaw length discrepancy in which one of the mandibles is shorter than the other, resulting in a shift of the mandibular midline (Figure 10), is typically a unilateral class II or III malocclusion.
Orthodontic problems arise from several different sources that can be genetic or nongenetic. In general, jaw length discrepancies (class II, III, and IV) are considered genetic (unless there is obvious evidence of a local or systemic cause) and tooth discrepancies (class I) are considered nongenetic. However, the increased incidence of lance effect in Shetland sheepdogs and base narrow in standard poodles makes a genetic component likely in these cases.
Managing deciduous dentition malocclusions
Most malocclusions can be diagnosed early, since they are often present in the deciduous dentition. An oral examination will reveal that the mandible and maxilla do not rest in the correct occlusion.
Depending on the class of malocclusion, palatine, gingival, or lip trauma may occur.5 The deciduous teeth (especially cuspids) are sharper than permanent teeth, so trauma and pain caused by deciduous teeth are more intense and are more likely to be clinically evident than that caused by permanent teeth. Patients with malocclusions often show no outward signs of distress. Regardless of the lack of clinical signs, if occlusal trauma is present, expedient therapy is mandated.
In some cases, the patient may be genetically programmed for a normal bite and have only a temporary malocclusion. Temporary malocclusions can occur since the maxilla and mandible may grow at varying rates during development because of an independent mandible or maxilla growth surge.4
When the deciduous dentition is trapped by a tooth or the soft tissues on the opposite arcade, it may interfere with the jaw movement and subsequent self-correction. This condition is called an adverse dental interlock (Figure 11).2
If occlusal trauma is present (Figure 12), extract the offending deciduous teeth expediently to minimize damage and discomfort.5 Even in the absence of occlusal trauma, extract the deciduous teeth to remove the adverse dental interlock and allow unrestricted jaw movement. This technique is the most common interceptive orthodontic procedure and should be performed as soon as the problem is noted (6 to 8 weeks of age) to allow the largest amount of normal jaw lengthening.5

Deciding which teeth to extract can be difficult. Obviously any tooth that is creating trauma should be extracted. When performing pure interceptive orthodontics, extract the teeth of the jaw that needs to grow, but make sure to remove any hindrance to movement.5
Managing permanent dentition malocclusions
If a problem does not self-correct, several options for therapy are available, depending on the presentation. Almost any orthodontic problem can be camouflaged with an orthodontic appliance. However, there are important ethical concerns about orthodontic therapy in animals.2,7 First, you must inform the client that most orthodontic problems are genetic in origin and that correcting the bite will not correct the genes. In addition, most orthodontic cases are cosmetic only, and subjecting a patient to the discomfort of an orthodontic appliance for the client's vanity may not be ideal. Finally, when the malocclusion is causing trauma, orthodontic therapy requires numerous anesthetic episodes, and other options may require only one procedure.
Class I malocclusions. Base narrow occurs when the mandibular cuspids exhibit linguoversion and cause palatine or gingival trauma (Figure 13). Intervention is critical in these cases. Options for therapy include moving the tooth orthodontically by removing a wedge of gingival tissue, placing composite crown extensions on the mandibular cuspids, or applying an incline plane (Figure 14). In addition, some dentists use ball therapy, which is inexpensive and noninvasive.9

If the owner wants one-step therapy, the offending area of the tooth can be removed. This is best achieved by coronal amputation and vital pulp therapy (Figure 15). When performed skillfully, this procedure enjoys an excellent success rate.10 However, the client must be cognizant of the need for follow-up radiographs. Also, some success has been seen with surgical movement of the tooth.11
Finally, the tooth may be extracted. Because of the size of the tooth and the importance of the mandibular cuspids in tongue retention and aesthetics, this is generally not the treatment of choice.2
Class II malocclusions. These malocclusions cause marked pain and inflammation that result secondary to the palatine trauma. Treatment of this condition is best achieved with coronal amputation and vital pulp therapy.
Mild cases can be treated orthodontically with a variant of an incline plane, but it is much more difficult to apply this in patients with class II malocclusions than in patients with base narrow malocclusions because of the trapping of the mandibular cuspids palatal to the maxillary cuspids. Severe cases can also be treated orthodontically by moving the mandibular cuspids into position distal to the maxillary cuspids. Finally, the tooth may be extracted.
Class III malocclusions. These malocclusions are generally only cosmetic and require no therapy. Orthodontic correction can be performed, but it is not recommended. In addition, it should be done only after strict genetic counseling. In rare cases, there may be maxillary lip trauma from the mandibular cuspids (especially in cats). In these cases, coronal amputation and vital pulp therapy or extraction can be performed.
MISSING TEETH
The eruption of the permanent dentition occurs within a fairly short time. Most breeds follow standard eruption times (Table 1), but some breeds have normally delayed eruptions. Teeth that have not erupted by the normal time (as defined by texts or by context of the eruption of the surrounding or contralateral teeth) should be considered pathologic. Patients most commonly have an abnormal space in the normal arcade (Figure 16A). Occasionally, however, a deciduous tooth will be intermixed in the permanent dentition (Figure 16B).
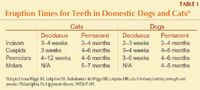
Table 1. Eruption Times for Teeth in Domestic Dogs and Cats*
Possible causes of missing teeth (i.e. teeth that do not erupt) include
1. Congenital: This abnormality is generally considered to be a genetic problem but can be secondary to in utero or neonatal problems. It is common in small, toy, and brachycephalic dog breeds. No specific therapy is necessary in these cases, but the patient should not be bred if a full dentition is standard.
2. Previously exfoliated: This condition is rare in juvenile patients, but it is possible. In these cases, radiographs will usually reveal evidence of a healing alveolus. Again, no specific therapy is necessary.
3. Fractured below the gingival margin: This condition is also rare in juvenile patients but common in adults. Dental radiographs will confirm a retained root (Figures 17A & 17B). If the root appears relatively normal (i.e. it is not being resorbed), surgical extraction is generally recommended to avoid pain and endodontic infection. If the tooth is showing marked resorption and no evidence of infection (periapical lucency), it can be radiographically monitored.

4. Impacted: Any tooth that remains unerupted beyond its normal eruption time is considered impacted.12 These teeth can be malformed or normal but do not erupt into the dentition because they are blocked by a structure such as bone or tooth (deciduous or permanent) or most commonly by an area of thick and firm gingiva called the operculum.4 This condition most commonly involves the first and second premolars of brachycephalic dogs. If caught early (before root end closure), removing the offending structure may allow the tooth to erupt normally. This procedure is called an operculectomy. Dental radiographs will confirm the unerupted tooth (Figures 18A & 18B).
The biggest concern with impacted teeth is the development of odontogenic cysts. These cysts originate from the enamel-forming organ of the unerupted tooth. The incidence of cyst development is unknown in veterinary medicine, but pathologic changes were noted in 32.9% of cases in one human study.13 In some cases, the cysts grow quickly and cause bone loss by pressure (Figure 19). This may result in a pathologic fracture. In addition, cysts can become infected and create marked swelling and pain. Finally, malignant transformation has occurred in some cases.14

Therapy for impacted teeth is surgical extraction. If cyst formation has occurred, en bloc removal or extraction of the tooth and meticulous curettage of the lining will prove curative.
Note that two of the causes of missing teeth require no therapy and that the other two can lead to serious pathology. So radiograph all missing teeth to ensure that they are truly missing.
ENAMEL HYPOCALCIFICATION
Enamel is a thin (< 1 mm) material on the surface of teeth.15 It is deposited on the dentin of the developing tooth by the enamel-forming organ. Enamel is only formed before tooth eruption and cannot be naturally repaired after eruption into the mouth. Hypocalcification results from a malformation of the enamel during its development. The malformed enamel will be easily lost, exposing the underlying dentin.
Causes
The most frequent cause of enamel hypocalcification in veterinary patients is trauma imposed on the unerupted tooth. This trauma is most commonly associated with the extraction of a deciduous tooth. In these cases, only one or several adjacent teeth will be affected. Other causes of this pattern of enamel hypocalcification include infection or inflammation from an overlying deciduous tooth.6
A severe infectious or nutritional problem may also result in improper enamel production. In these cases, most or all of the teeth are affected but only in a small part of the crown, usually a horizontal circumferential strip.6 Canine distemper was a common cause of this condition in the past.2 Improper enamel production may also result from a hereditary decrease in the amount of enamel matrix applied to the teeth during development.12 This condition is known as amelogenesis imperfecta. In these cases, almost all teeth on almost all surfaces are involved.
Diagnosis
Regardless of cause, the areas of weakened enamel will flake off and expose the underlying dentin. Dentin is a porous material and becomes stained easily. Consequently, areas of enamel hypocalcification will generally appear tan to dark-brown and pitted and rough (Figure 20). The tooth surface is hard, however, as opposed to the soft and sticky surface of caries.
The dentinal exposure will result in marked discomfort for the patient.6 Each square millimeter of crown surface contains 45,000 dentinal tubules, each of which communicates with the root canal system. Dentin exposure will change the fluid dynamics within the dentinal tubules. The change in fluid velocity within the tubules is translated into electrical signals by the sensory fibers located within the tubules or subjacent odontoblast layer. These signals result in the sensation of pain (or sensitivity) within the tooth.16 It is rare for veterinary patients to exhibit this discomfort, but occasionally anorexia will result. These exposed dentinal tubules can also act as a conduit for bacterial infection of the root canal system. The tooth surface roughness results in increased plaque retention, which speeds the onset of periodontal disease. For all of these reasons, promptly treating these teeth is critical.
In cases of widespread hypocalcification, it is common to find malformed roots as well; many times there is little root structure (Figure 21). While endodontic infection of these roots is rare, the lack of root structure will result in early exfoliation secondary to trauma or periodontal disease.

Treatment
Treatment is aimed at removing sensitivity and avoiding endodontic infection by occluding the dentinal tubules as well as smoothing the tooth to decrease plaque accumulation. The most efficient and aesthetic way to accomplish these goals is to place a bonded composite restoration (Figure 22). This procedure is performed by removing the diseased dentin with a diamond or finishing dental bur or polishing disk. Next, a commercial bonding agent is applied, and a composite resin is placed and roughly shaped to natural tooth contours and then light-cured. The restoration is then shaped and smoothed with a diamond bur or sanding disk. Finally, a coat of unfilled resin is applied for optimum smoothness and shine. In very small teeth, the unfilled resin alone may be sufficient.
If the damage is severe and the client is interested in a permanent correction, crown therapy can be performed. Alternatively, extraction may be performed, but this is not the recommended course of therapy if the tooth has a normal root structure and no evidence of endodontic infection.
ORAL PAPILLOMATOSIS
These papillomas are most commonly induced by a papovavirus, but they can be idiopathic.17 They are usually transmitted by direct contact, but indirect contact may also be sufficient. There is generally a two- to six-month incubation period.18 These papillomas are most commonly seen in young dogs as white, gray, or flesh-colored masses on the oral mucosa (Figure 23). They can be solitary or multiple lesions spread throughout the mouth on the palate, tongue, or oropharynx. The papillomas are usually pedunculated or cauliflower-shaped. Size may range from a few millimeters to a few centimeters.18
Treatment
Viral papillomas are generally self-limiting and will resolve over a period of weeks to months. Typically, no therapy is required. After regression, patients are generally immune to reinfection.19 However, there are reasons to initiate therapy in suspected cases of papillomatosis. First, the papillomas can become infected, which may result in marked local inflammation. Also, they can mimic more aggressive tumors, and, finally, malignant transformation has been reported.20
Consider surgical removal or debulking with histologic analysis in patients in which the masses are severely infected or are large and interfere with mastication.12 In addition, histology (ideally excisional) should be pursued if the growths are not regressing or look atypical. Excision can be performed with a standard surgical approach, cryosurgery, electrosurgery, or laser therapy.
Additional therapeutic measures in persistent cases include vaccination, traumatic crushing, and chemotherapy.12 However, vaccination has not proved particularly successful, and squamous cell carcinomas have been reported to arise at the injection sites.21
Brook A. Niemiec, DVM, DAVDC
Southern California Veterinary Dental Specialties
5610 Kearny Mesa Road, Suite B1
San Diego, CA 92111
REFERENCES
1. Bellows JE, Dumais Y, Gioso MA, et al. Clarification of veterinary dental nomenclature. J Vet Dent 2005;22:272-279.
2. Harvey CE, Emily PP. Occlusion, occlusal abnormalities, and orthodontic treatment. In: Harvey CE, Emily PP, eds. Small animal dentistry, St. Louis, Mo: Mosby, 1993;266-296.
3. Wiggs RB, Lobprise HB. Oral anatomy and physiology. In: Wiggs RB, Lobprise HB, eds. Veterinary dentistry: principles and practice. Philadelphia, Pa: Lippincott–Raven, 1997;55-86.
4. Wiggs RB, Lobprise HB. Pedodontics. In: Wiggs RB, Lobprise HB, eds. Veterinary dentistry: principles and practice. Philadelphia, Pa: Lippincott–Raven, 1997;167-185.
5. Hale FA. Juvenile veterinary dentistry. Vet Clin North Am Small Anim Pract 2005;35:789-817.
6. Neville BW, Damm DD, Allen CM, et al. Abnormalities of teeth. In: Oral and maxillofacial pathology. 2nd ed. Philadelphia, Pa: Saunders, 2002;49-106.
7. Wiggs RB, Lobprise HB. Basics of orthodontics. In: Wiggs RB, Lobprise HB, eds. Veterinary dentistry: principles and practice. Philadelphia, Pa: Lippincott–Raven, 1997;435-481.
8. Bellows J. Atlas of canine dentistry: malocclusions and breed standards. Waltham publication.
9. Verhaert L. A removable orthodontic device for the treatment of lingually displaced mandibular canine teeth in dogs. J Vet Dent 1999;16:69-75.
10. Niemiec BA, Mulligan TM. Assessment of vital pulp therapy for nine complicated crown fractures and fifty-four crown reductions in dogs and cats. J Vet Dent 2001;18:122-125.
11. Amimoto A, Iwamoto S, Taura Y, et al. Effects of surgical orthodontic treatment for malalignment due to the prolonged retention of deciduous canines in young dogs. J Vet Med Sci 1993;55:73-79.
12. Wiggs RB, Lobprise HB. Clinical oral pathology. In: Wiggs RB, Lobprise HB, eds. Veterinary dentistry: principles and practice. Philadelphia, Pa: Lippincott–Raven, 1997;104-139.
13. Raghoebar GM, Boering G, Vissink A. Clinical, radiographic, and histological characteristics of secondary retention of permanent molars. J Dent 1991;19:164-170.
14. Neville BW, Damm DD, Allen CM, et al. Odontogenic cysts and tumors. In: Oral and maxillofacial pathology. 2nd ed. Philadelphia, Pa: Saunders, 2002;589-642.
15. Crossley DA. Tooth enamel thickness in the mature dentition of domestic dogs and cats—preliminary study. J Vet Dent 1995;12:111-113.
16. Pashley DH, Liewehr FR. Structure and functions of the dentin-pulp complex. In: Cohen S, Hargreaves KM, eds. Pathways of the pulp. 9th ed, Philadelphia, Pa: Mosby, 2006;460-513.
17. Gross TL, Ihrke PJ, Walden EJ. Epidermal tumors. In: Veterinary dermatopathology. St. Louis, Mo: Mosby-Year Book, 1992:330-350.
18. Scott DW, Miller WM, Griffin CE. Neoplastic and non-neoplastic tumors. Cutaneous papilloma. In: Muller & Kirk's small animal dermatology. 5th ed. Philadelphia, Pa: WB Saunders Co, 1995;994-999.
19. Harvey RG, McKeever PJ. Nodular dermatoses. In: A colour handbook of skin diseases of the dog and cat. London: Manson Publishing, 1998;57-59.
20. Watrach AM, Small E, Case MY. Canine papillomas: progression of oral papilloma to carcinoma. J Natl Cancer Inst 1970;45:915-920.
21. Bregman CL, Hirth RS, Sundburg JP, et al. Cutaneous neoplasms in dogs associated with canine oral papillomavirus vaccine. Vet Pathol 1987;24:477-487.